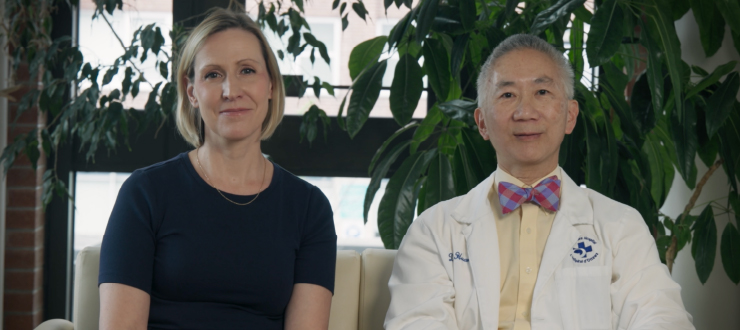
Debi Lascelle (left) and Stephen Aronson are patient advisors on a lung screening pilot program. Both Lascelle and Aronson were diagnosed with lung cancer and treated successfully after taking part in an early screening study.
When people found out that Debi Lascelle had been diagnosed with lung cancer, they almost always reacted the same way.
“Most of them would say, ‘Well, did you smoke?’ I try to own it and say, ‘Yes, I did. Next question?’”
Her cancer was diagnosed in 2011 when she took part in a study about lung screening. At the time, she was training to volunteer at the May Court Hospice.
“My dad died of lung cancer. So when I saw the ad for the study, I carried it around for a while, thinking about it, and then I called,” she said.
Family history was also on Stephen Aronson’s mind when he registered for the same study and was diagnosed with lung cancer.
“My father was a smoker, and his father was also smoker. My father had lung cancer and he ended up dying of it in the ‘90s,” he said.
Lung cancer is the leading cause of cancer death for women and men in Ontario. About 7,100 people died of lung cancer in 2016 – more than breast, colorectal and prostate cancers combined.
Regular lung screening for people at a high risk of lung cancer isn’t standard practice in Ontario. For both Aronson and Lascelle, screening meant that their cancers were found at a more treatable stage.
The Champlain Regional Cancer Program, based at The Ottawa Hospital, is one of three regions in the province taking part in a Cancer Care Ontario program to pilot screening for people at a high risk of lung cancer. Lascelle and Aronson are patient advisors for the pilot at The Ottawa Hospital and Renfrew Victoria Hospital.
“The chance of someone surviving lung cancer has not improved very much over the last few decades,” said Dr. Donna Maziak, a surgical oncologist and the physician lead for the program. “We wanted to pilot this program because we think that combining lung screening with smoking cessation will improve the odds for our patients. It will give us a new weapon in our fight against lung cancer.”
The program launched June 1. People between the ages of 55 and 74 who have smoked for 20 or more years – not necessarily consecutive years – are considered to be at a high risk of developing lung cancer, and might be eligible.
For Dr. Treena Greene, Aboriginal Cancer Lead at The Ottawa Hospital, there are clear benefits for screening.
“I have had to say goodbye to my grandfather and my husband’s ataatatsiaq [maternal grandfather], who both died from lung cancer,” she said. “I need you to ask about lung cancer screening. Taking the time now could give you more years with your loved ones.”
Aronson quit smoking for good before he got his diagnosis, but, “it’s like with any addiction. You may have quit, but you’re still a smoker,” he said. By acting as a patient advisor for the program, he said, he’s able to address some of the stigma directly.
Lascelle agreed. “Attitudes towards smoking have changed a lot, but I was around smokers my whole life. Everyone in my family smoked. I took it up at 14 and quitting was the hardest thing I’ve ever done.”
Everyone referred to the program will be offered support to quit smoking. If you or someone you know would like to learn more about quitting or reducing smoking, visit www.myquit.ca, or call 1-877-376-1701.

Support patient care and research at
The Ottawa Hospital
You might also like…
Less time charting means more time with patients: How The Ottawa Hospital is using AI to support patient care
“I’m seeing and treating more patients.” Find out how DAX Copilot, a powerful AI assistant, is helping our physicians cut down on paperwork, improve their own well-being and spend more time with patients.
Aging well: Guidance for older adults
In this special video series for both older adults and their loved ones, geriatric care specialists from The Ottawa Hospital offer guidance on navigating common health-care challenges that may arise with aging.
How to stay safe around water this summer
Drowning can happen to anyone — even strong swimmers. Emergency physician Dr. Christian Vaillancourt debunks common myths about drowning, explains how to act quickly to save a life, and shares what you can do to keep yourself and your loved ones safe around water.
What’s the difference between an optician, optometrist, orthoptist and ophthalmologist?
“Do I need to see an optician, optometrist, orthoptist or ophthalmologist?” We asked Ophthalmologist Dr. Annick Fournier to break down each role so you will know who to consult for your specific eye care needs.
New reusable surgical gowns a step towards greener operating rooms
The Ottawa Hospital is finding safe, innovative ways to reduce medical waste in its operating rooms by using more environmentally sustainable products.
Understanding rabies: Risks, vaccination and what to do after a bite
Although rare in Canada, rabies is almost always fatal once symptoms appear. Infectious diseases expert Dr. Michaeline McGuinty shares how rabies is spread, when to get vaccinated and what to do after a bite.


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.