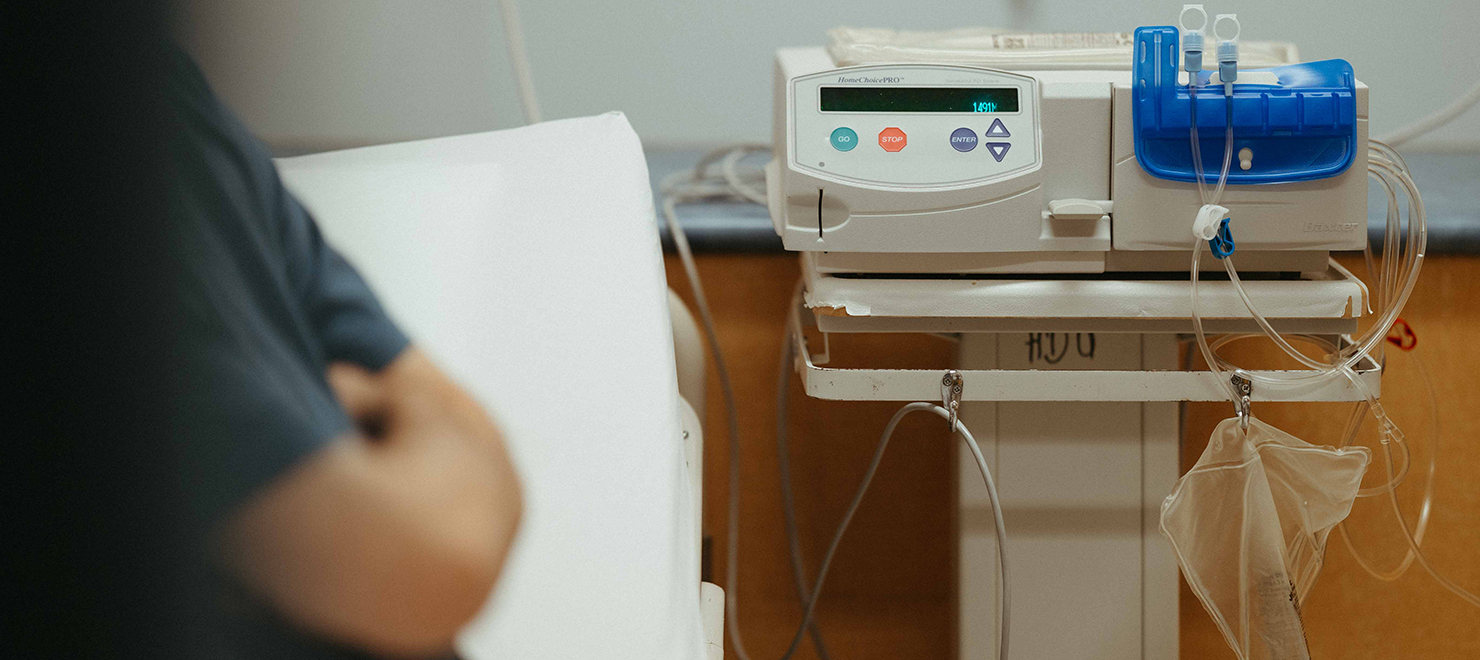
For people in our community living with kidney failure, regular dialysis treatment is a reality. Dialysis helps filter toxins, waste and excess fluid out of the bloodstream when the kidneys aren’t working properly.
The most ideal form of dialysis treatment is done in the home, rather than at a hospital or dialysis centre. This provides more flexibility in patients’ schedules, putting more time back in their days to do the things they love.
In May of 2018, The Ottawa Hospital significantly redesigned and expanded the Home Dialysis Program, making it more accessible to more patients—and turning it into a model for home dialysis programs across the province.
Here’s how we made it happen.
A new model of care
First, some context.
Currently, more than 230 patients are enrolled in The Ottawa Hospital’s Home Dialysis Program. The most common form of dialysis performed at home is peritoneal dialysis, which is done by infusing a special fluid in the abdomen through an abdominal catheter, cleaning the blood of toxins and allowing for fluid and waste removal.
All our home dialysis patients receive one-on-one training on how to manage their condition from home and how to use dialysis equipment. But some patients need a bit of extra help.
Before 2018, if any of our peritoneal dialysis patients required support at home, we would refer them to the Champlain Community Care Access Centre, now known as Home and Community Care Support Services Champlain, which would dispatch nurses to help patients in need.
Today, if a peritoneal dialysis patient isn’t well enough or doesn’t feel comfortable using their dialysis machine, our nurses will visit the patient at their home, once before bedtime to connect them to the unit and again in the morning to take them off.
“I looked at our entire program and redesigned it to incorporate home care into the day-to-day work of our home dialysis staff,” explains Janet Graham, Regional Director of Nephrology at The Ottawa Hospital. “We hired more staff and provided more education about caregiving in the home.”
The Ottawa Hospital no longer relies on Home and Community Care Support Services’ resources to support peritoneal dialysis care for patients in their home. We are now the only home peritoneal dialysis provider in the city.

Enhancing quality of life for our patients
In the past, peritoneal dialysis patients would need to be fully trained before they went home from the hospital. But with more staff members on board, patients can receive training and support in their homes the same day they’re discharged—and they can be discharged faster. “If we have a patient who is now ready to go home at noon, I can have a nurse meet them at home by the time they get there,” says Janet.
Fewer patients also require re-admission to the hospital. Our staff members are very attuned to the specific needs of their patients, as the same nurses who patients see at clinic appointments also train and care for them at home. “Innovating the program has enabled us to provide significant continuity of care,” says Janet.
This continuity of care coupled with ongoing education has had a profound impact on patients’ lives. “We’ve been very successful at transitioning many patients away from fully assisted home dialysis to full independence.”

Inspiring home dialysis programs across the province
Our Home Dialysis Program is the first in Ontario to have hospital staff members provide home care, as opposed to relying on third-party agencies. During the pandemic, many of these agencies found themselves short of staff, leaving many peritoneal dialysis patients without dialysis care in their homes.
That wasn’t the case for our patients.
“We managed to make it through the entire pandemic seamlessly,” Janet reports with pride. “We were so successful during COVID and throughout the past five years that the Ontario Renal Network has described the model we’ve designed as ‘the Ottawa model.’ And now, other home dialysis programs in Ontario are looking to us to figure out how they can do the same thing.”
Expanding care to more dialysis patients
Currently, the Home Dialysis Program provides assisted care in the home to peritoneal dialysis patients only. The program has always provided critical training to home hemodialysis patients, helping them achieve independence, but our team does not provide assisted care in the home.
Janet plans to change that.
“We want to provide our home hemodialysis patients with the same support we’re providing our home peritoneal dialysis patients,” says Janet. “And we’re working with the Ontario Renal Network to make that happen.”
The Ontario Renal Network wants to expand home dialysis throughout the province—and The Ottawa Hospital’s Home Dialysis Program is helping to achieve that goal. “We certainly have grown, and we continue to grow,” says Janet. “By having patients at home, in the place where they are most comfortable, we can significantly improve their quality of life.”
Strong staffing allowed the program to grow by seven new home dialysis patients over the past 18 months, while across the province, the number of patients on home dialysis decreased by 177 during that same period.

A provincial leader in kidney transplants
“I am proud that The Ottawa Hospital has transplanted a lot of people who’ve been on home dialysis,” Janet reports with a smile.
Of all the large dialysis programs in the province, The Ottawa Hospital has the highest rate of patients (both home patients and in-centre patients) who go on to receive transplants. More than half of our home dialysis patients are either on the transplant list or are in the process of being listed.
The Ottawa Hospital also has a well-established and innovative Living Kidney Donor program. To learn about living kidney donation and read inspiring stories from donors and recipients, we invite you to visit our Living Kidney Donation website.
And for more information about home dialysis and our program, please visit our Home Dialysis Program webpage.

Support patient care and research at
The Ottawa Hospital
You might also like…
Dr. Kathleen Gartke appointed to the Order of Ontario
The Ottawa Hospital is proud to share that Dr. Kathleen Gartke has recently been appointed to the Order of Ontario, the province’s highest honour. A pioneering orthopedic surgeon, Dr. Gartke has been recognized for advancing patient care and women’s leadership in medicine.
Reimagining hospital food: How The Ottawa Hospital is transforming the patient mealtime experience
In 2024, we launched the trial phase of our Patient Food Transformation Project. The goal was to see if it is possible to improve the overall nutrition and quality of food we serve to our patients, while increasing bedside hospitality, enhancing the overall sustainability of our food services, and not increasing operational costs. Our trial wrapped in 2025 with very promising results.
How we’re helping over 1,400 paramedics enhance patient care and safety
The Regional Paramedic Program for Eastern Ontario (RPPEO) is on a mission to enhance what happens after you dial 911. Here are three new ways this team is helping paramedics deliver better, safer care to their patients.
New program fills gap in care for teens and young adults with cancer
For young people, a cancer diagnosis can disrupt their education, careers, relationships and family-building goals. Our Adolescent and Young Adult (AYA) Cancer Program supports AYAs on their cancer journey, complementing the care provided by their care team.
OnTrack program helps young adults experiencing psychosis find their footing
A unique program run by The Ottawa Hospital is celebrating 20 years of providing care and support to young adults navigating their first episode of psychosis.
Less time charting means more time with patients: How The Ottawa Hospital is using AI to support patient care
“I’m seeing and treating more patients.” Find out how DAX Copilot, a powerful AI assistant, is helping our physicians cut down on paperwork, improve their own well-being and spend more time with patients.


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.





