Do you feel unstable on your feet? How about your parents or someone you know? Even fit, independent adults can be at a greater risk of falling because for many, the COVID-19 pandemic and subsequent public health guidelines had the unintended effect of decreasing a person’s overall activity.
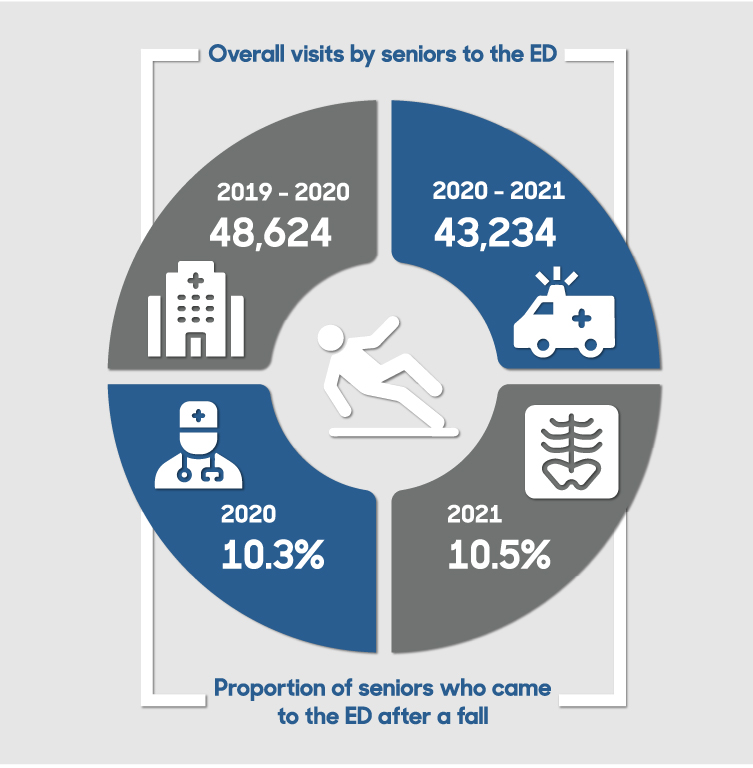
Data from The Ottawa Hospital show that although fewer seniors came to our emergency departments (ED) overall, more seniors came because of a fall.
Why? Likely because of decreased activity. For example, some older adults opted for curb-side pickup or grocery delivery rather than walking around the grocery store. Many social engagements that would have increased overall activities were cancelled. For older people especially, less general activity leads to weaker muscles and poorer balance, which in turn can lead to more falls.
Based on these trends, the hospital expects more seniors to come to the emergency department in 2022 after a fall. That’s because as public health restrictions lift, seniors who have not been active for the past 18 months will start being more active again and more willing to come to the emergency department for care after a fall.
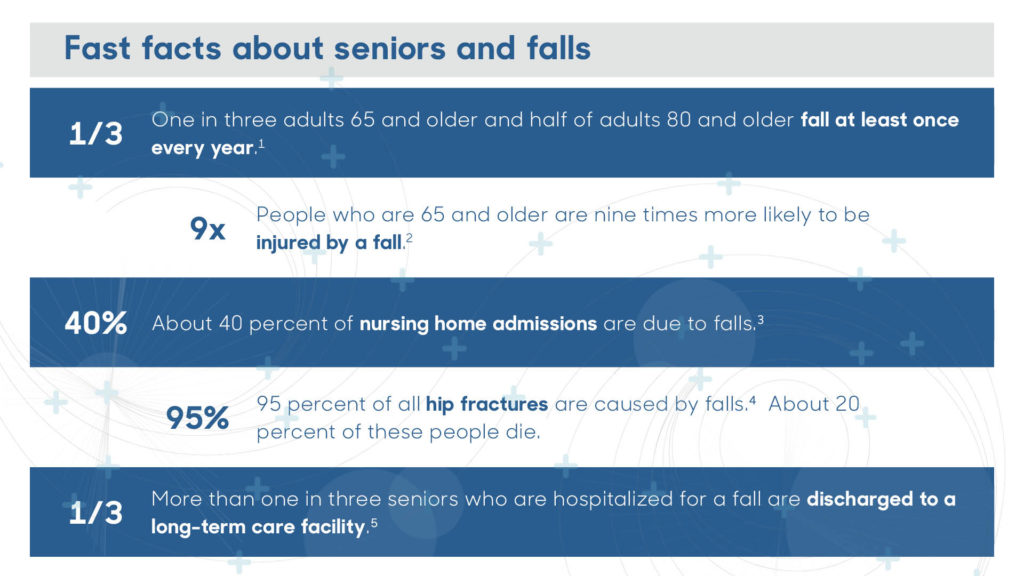
Facts about seniors and falls
- One in three adults 65 and older and half of adults 80 and older fall at least once every year. [1]
- People who are 65 and older are nine times more likely to be injured by a fall. [2]
- About 40 percent of nursing home admissions are due to falls. [3]
- 95 percent of all hip fractures are caused by falls. [4] About 20 percent of these people die.
- More than one in three seniors who are hospitalized for a fall are discharged to a long-term care facility. [5]
Not sure of your fall risk? Check your risk with the staying independent checklist.
Falls do not have to be a normal part of aging. In fact, studies suggest that many falls are preventable.
If you’re a senior or care for one who is, follow these fall prevention tips.
How seniors can prevent falls
Exercise, exercise, exercise
Being active is one of the best ways to prevent falls because regular physical activity and exercise improves balance and muscle strength.

Health Canada recommends 150 minutes of moderate to vigorous activity every week, and strength and balance activities at least twice per week. If you haven’t been active in a while, increase your activity gradually. Be sure to talk to your health-care provider before you start a new exercise program to make sure that it is right for you.
Know your medications
In general, the more medications you take, the greater your risk of falling.
As you age, medications can affect your body in new ways. Keep a current list of medications with you and in your home. It’s also really important to use only one pharmacy so that the pharmacist knows all the medications that you take.
Remember to review your medications (including over-the-counter and natural health products) with your doctor or pharmacist. Ask how alcohol or cannabis might affect your medications and tell them if you are concerned about your medications and their side effects.
Why do falls matter?
Falls can result in serious injuries such as brain trauma and bone fractures. They can also cause chronic pain, make it harder to move around, and reduce independence. Some falls can cause depression and even death.
One bad fall can cause an otherwise healthy person to become frail and less active, which in turn can further increase their chances of falling.
Keep your home safe
Fifty percent of falls occur at home, so use a checklist to identify fall risks. Scatter rugs, loose railings, poor lighting and floor clutter are examples of things that can all increase your chances of falling.
Remember to ask for help with tasks that you feel you can’t do safely.
Care for your eyes and ears
Vision changes as people age. It is harder for seniors to judge distance and depth. Depth perception helps us go up and down stairs and curbs safely, so poor depth perception can lead to a fall.
Use caution if you have multifocal lenses like bifocals or progressives because these kinds of lenses can increase the risk of falling. The prescription at the bottom of the lens is meant for reading, not looking at the ground, so these kinds of glasses can alter depth perception and cause the wearer to misjudge the height of a step, for example.
Older adults are also more sensitive to glare, and they need more light to see at night. In fact, people who are 60 years old need ten times more light to see at night than teenagers. It also takes their eyes longer to adjust to sudden light changes.
How well a person hears can also affect their chances of falling. Research has found that people with hearing loss are three times more likely to fall than people without hearing loss.
So remember to get your vision and hearing tested every ear, and wear any prescribed glasses and hearing aids.
Consider a walking aid
A walking aid such as a cane, walker or walking poles can help prevent falls by helping you feel more stable and comfortable. It can also increase your endurance and reduce pain on your joints.
Would a walking aid help me?
Here are some questions to ask yourself:
- Am I concerned about my balance?
- Am I reaching for furniture or walls for support?
- Do I have trouble stepping up a curb?
- Do I have leg pain that affects my walking?
If you answered yes to any of these questions, you may benefit from a walking aid. Talk to your health-care provider.
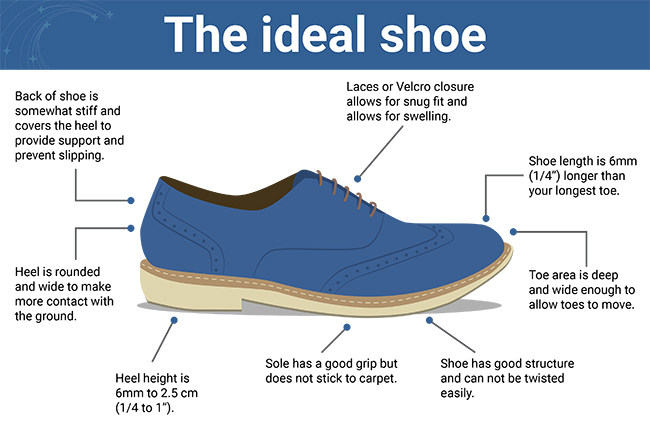
Wear safe shoes
Well-fitting and supportive shoes are a great addition to your wardrobe. They can make you feel more stable and comfortable, protect your feet and lessen the impact on your joints. The best options are closed-toe, have low heels and have non-slip soles.
Be winter ready
Slippery surfaces can greatly increase your risk of falling. Make sure your walkways, stairs and driveway are clear of ice and snow. Put on boots with a wide, low, non-slip heel before going outside. If you use a cane, consider adding a retractable ice pick for extra grip. Carry a bag of grit, sand or cat litter in your pocket that you can sprinkle on icy surfaces if needed.
Check Rate My Treads from the Kite Research Institute for a list of recommended footwear and slip resistance ratings.
See your health-care team
Tell your health-care provider if you are concerned about your balance or are having trouble walking steadily. It is also important to share any times you have
- felt dizzy
- felt drowsy
- lost consciousness, even for a moment, or
- felt pain that is affecting your ability to be active
They can help identify possible reasons for the fall and together you can come up with a plan.

What to do if you fall
- Don’t rush to get up. Make sure you’re not injured before trying to move.
- If you think you can get up, turn onto your hands and knees and crawl to stable furniture to help you.
- If you cannot get up, call for help. If you have an emergency call device or telephone within reach, use it.
- Don’t let the fear of falling again stop you from being active. Inactivity creates an even greater risk of falling.
Learn more about what to do after a fall.
Remember, falls do not have to be a normal part of aging. If you notice a change in your balance, strength, or mobility, talk to your health-care team. It is much better to take steps to prevent falls than manage the health outcomes after you fall.
About The Ottawa Hospital’s Falls Assessment Clinic
The Champlain Falls Assessment and Streamlined Treatment (C-FAST) Clinic at The Ottawa Hospital is a specialized clinic for patients who are at risk of falls. Held Monday and Thursday afternoons, clinic staff typically see about 140 patients per year.

Patients who are referred to the clinic are assessed by an advanced practice nurse, a physiotherapist, a geriatrician and a pharmacist (when required) during a three-hour appointment. During the COVID-19 pandemic, the first part of the assessment is done virtually by phone or secure video chat to shorten the time patients spend in the clinic.
Patients can expect a “multifactorial” assessment, which means that the professionals look at each patient’s fall risk factors within their area of expertise and offer evidence-based recommendations to reduce them.
The geriatrician will diagnose and treat any relevant medical issues that may contribute to fall risk. They may change a patient’s medications or order tests such as bloodwork, x-rays, bone mineral density tests and CT scans. Other recommendations may include incorporating a gait aid such as a walker or canes, using a personal alarm system or changing footwear.
Clinic staff connect patients with resources to help meet their unique needs, such as a community-based exercise program (virtual or in-person) and a home safety assessment. Staff also follow up with patients by telephone to see how well they are following the recommendations and offer more help if needed. Most of all, the clinic staff want all patients to feel welcome and provide hope that they can take action to prevent falls and live a healthy life.
Early intervention keeps seniors independent longer
By seeing patients early in their ‘falls history’ the team helps them modify their risk factors, which can help reduce the number of falls and fall-related injuries. Avoiding falls means seniors can stay independent longer and lessens the chances of needing to go to the ED or be admitted to the hospital due to injuries from a fall.
Family doctors can consider referring their at-risk older adult patients to Specialized Geriatric Services – Central Intake for an assessment at the C-FAST clinic or other specialized programs in the region.
[1] Public Health Agency of Canada Seniors Falls in Canada Report 2014.
[2] Scott, V. (2012). Fall Prevention Programming: Designing, Implementing and Evaluation Fall Prevention Programs for Older Adults.
[3] Scott, V. (2012). Fall Prevention Programming: Designing, Implementing and Evaluation Fall Prevention Programs for Older Adults.
[4] Parkkari J, Kannus P, Palvanen M, Natri A, Vainio J, Aho H, Vuori I, Järvinen M. Majority of hip fractures occur as a result of a fall and impact on the greater trochanter of the femur: a prospective controlled hip fracture study with 206 consecutive patients. Calcif Tissue Int, 1999;65:183–7.
[5] Public Health Agency of Canada Seniors Falls in Canada Report 2014.

Support patient care and research at
The Ottawa Hospital
You might also like…
Living with chronic pain? This online tool offers help — and hope
The Power Over Pain Portal is a free virtual resource hub designed to help empower youth and adults living with chronic pain through education and peer support.
What to do in an emergency: New first aid video series on YouTube
Would you know what to do if you saw someone experience a stroke, heart attack or opioid overdose? We’ve launched a series of easy-to-follow videos on YouTube that walk you through how to respond to common first aid emergencies.
Flu season 101: A quick guide to keeping the sniffles away
Got two minutes? This short guide could help you make it through flu season without stocking up on tissues.
Aging well: Guidance for older adults
In this special video series for both older adults and their loved ones, geriatric care specialists from The Ottawa Hospital offer guidance on navigating common health-care challenges that may arise with aging.
How to stay safe around water this summer
Drowning can happen to anyone — even strong swimmers. Emergency physician Dr. Christian Vaillancourt debunks common myths about drowning, explains how to act quickly to save a life, and shares what you can do to keep yourself and your loved ones safe around water.
What’s the difference between an optician, optometrist, orthoptist and ophthalmologist?
“Do I need to see an optician, optometrist, orthoptist or ophthalmologist?” We asked Ophthalmologist Dr. Annick Fournier to break down each role so you will know who to consult for your specific eye care needs.


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.