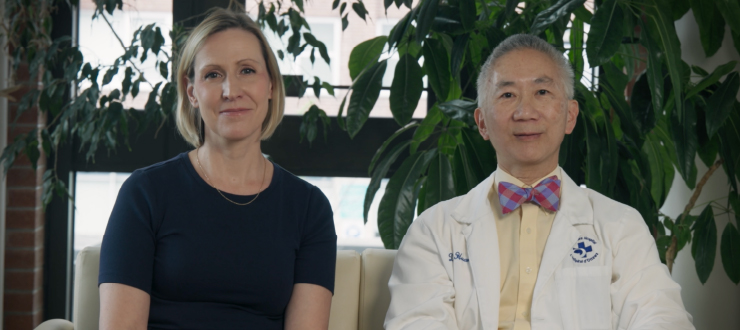
For years, Dr. Kumanan Wilson, senior scientist at The Ottawa Hospital and professor at the University of Ottawa, has researched immunization and using data to improve vaccine safety. Now, he’s focusing his work on the COVID-19 virus and newfound vaccines.
In 2020, the first COVID-19 vaccines were approved for use in Canada. With this exciting news, also comes questions about the vaccine’s safety, the process to get vaccinated and what happens after. We spoke to Dr. Kumanan Wilson, senior physician scientist at The Ottawa Hospital and professor at the University of Ottawa, to get answers to some of the most popular questions about the COVID-19 vaccines.
COVID-19 vaccine safety
Is the COVID-19 vaccine safe?
The short answer is yes. The vaccine has met safety standards in basic clinical trials and it’s also met safety standards outlined by Health Canada regulators. Additionally, the vaccine’s safety will continue to be monitored over the coming weeks and months as more members of the public get the vaccine.
Sometimes, as vaccines are monitored, safety signals arise that need further evaluation. As a result, the government may pre-emptively change recommendations for vaccines until further evidence becomes available. Such a scenario has unfolded with the Astra-Zeneca vaccine
How does the vaccine protect us against COVID-19?
There’s not just one vaccine, there are several vaccines. This is important to highlight because there could be many vaccines available and they all have a different way of working.
The cool thing about these messenger RNA (mRNA) and synthetic vaccines, like the Pfizer and Moderna vaccines for COVID-19, is that they give little recipes in the form of mRNA to our cells. The recipes then go into our cells and our cells make the spike protein which is then used to train the immune system to attack the virus.
Typically, vaccines train your immune system to recognize a part of the virus, usually a protein. If you’re exposed to the virus after getting vaccinated, your immune system is ready to immediately attack it using the adaptive immune response, that’s the body’s antibodies and T-cells.
The cool thing about these messenger RNA (mRNA) and synthetic vaccines, like the Pfizer and Moderna vaccines for COVID-19, is that they give little recipes in the form of mRNA to our cells. The recipes then go into our cells and our cells make the spike protein which is then used to train the immune system to attack the virus.
What are the potential side effects of the COVID-19 vaccine?
Common side effects are local reactions, like a fever or fatigue, and swelling or soreness where you got the injection. We’ve seen some people who received the COVID-19 vaccine have an anaphylactic reaction because they have allergies to some of the vaccine’s ingredients, but this is a very uncommon side effect. People with a history of severe allergies were excluded from the initial studies. As we continue studying the effects of the COVID-19 vaccine, clinics will ask you if you’ve had allergic reactions to other vaccines to ensure it’s safe for you to get.
Why do some people have side effects to a vaccine?
The most common side effects from a vaccination are usually signs that the vaccine is doing its job. When you feel some soreness, some swelling, some fatigue or a low fever, it means that the vaccine has triggered an immune response, which is exactly what we want it to do.
However, there is the possibility of side effects developing that were too rare to be detected in clinical trials. These require further evaluation to determine whether they are causally related to the vaccine and whether it is limited to specific batches.
What does percent efficacy mean in a vaccine?
Percent efficacy means the reduction in COVID-19 cases due to the vaccine, compared to the placebo in clinical trials. A vaccine efficacy of 50 percent indicates a 50 percent reduction in disease occurrence among the vaccinated group, or a 50 percent reduction from the number of cases you would expect if they have not been vaccinated. In a group of 100 vaccinated people, on average, only 50 people instead of all 100 people would get ill if all 100 were exposed to the virus.
All Health Canada approved vaccines have strong efficacy protecting against severe illness.
More information about the efficacy of the vaccines approved by Health Canada is available on the Ottawa Public Health website.
Why aren’t vaccines 100 percent effective?
The Pfizer COVID-19 vaccine has shown 95 percent effectiveness, and that’s incredible. Most of our vaccines don’t achieve that level of effectiveness – with the flu vaccine you’ll see 70, 80 and 90 percent effectiveness which is still really good. The 95 percent effectiveness of the mRNA vaccines is amazing.
It’s challenging to reach 100 percent effectiveness because some people’s immune systems don’t respond to the vaccine’s effects. This can sometimes happen in older adults whose immune systems aren’t as responsive, or in people who have conditions where their immune system doesn’t work as well.
Why were we able to find a vaccine for COVID-19 so quickly and get it approved?
It’s a great success story. Researchers were able to leverage a lot of the work that was already happening in the vaccine field, especially the research on mRNA vaccines. That technology had been tested on a bunch of other viruses and researchers were able to quickly shift focus once they had detailed information about the COVID-19 virus.
Finding the vaccine was a monumental effort for many reasons. Researchers were able to recruit thousands of people into large trials. Because COVID-19 was so widespread in communities around the world, they were able to get the sample sizes needed to power the trials and get a true picture of how the vaccine worked. These two factors sped up the process of finding a vaccine.
Why are there so many different types of COVID-19 vaccines in trial?
There are many different vaccines in trial because researchers didn’t know if any of them were going to work. We needed to shoot many bullets at the virus and hope some of them hit. So far, it’s been a remarkable story.
Making vaccines for viruses like this is a tricky business – we don’t even have a vaccine for the common cold virus. The idea was to engage all our vaccine developers and manufacturers, get all of them working on it, and hope that a vaccine might work. That’s the first part of the story.
The second part of the story is that even though we already have several successful vaccines, we still need more. The more vaccines we have available, the better we can leverage manufacturing capacity around the world to make enough vaccines to vaccinate the world’s population. Thanks in part to community support, researchers at The Ottawa Hospital are well-positioned to help with this global effort.
Why are some vaccines kept frozen or cold?
The mRNA in the Pfizer COVID-19 vaccine is fragile and can degrade. Keeping it cold prevents the degradation of the mRNA. Essentially, cold temperatures preserve the vaccine.
What is herd immunity? When would we achieve it?
Herd immunity is what happens when a certain percent of a community becomes immune to a virus and so the spread of the virus declines. When herd immunity is achieved, the whole community is protected from the virus, not just those who are immune.
The most common side effects from a vaccination are usually signs that the vaccine is doing its job. When you feel some soreness, some swelling, some fatigue or a low fever, it means that the vaccine has triggered an immune response, which is exactly what we want it to do.
While experts don’t know what percentage of people would need to get vaccinated to achieve herd immunity to COVID-19 just yet, some estimates suggest it may be around 60 to 70 percent. At this point, the virus would start running into too many people who have been immunized against it, and its ability to spread would slow down and eventually stop. The fastest way to reach herd immunity is through mass vaccinations, which is happening as we speak.
Vaccination
Who gets a COVID-19 vaccine first? How is that decided?
In Canada, the National Advisory Committee on Immunization (NACI), which is an independent expert advisory committee on vaccines, has been tasked with providing recommendations on the order in which people will have access to the vaccine. The committee is made up of vaccine experts from around the country who have looked at the available research to make recommendations on the use of the COVID-19 vaccines. Ultimately, the provinces will decide how the vaccine is distributed, but they usually follow the guidance of the NACI because many of the committee’s members work directly with the provinces.
Right now, the COVID-19 vaccination guideline in Canada is to vaccinate the most vulnerable people first, and then vaccinate those who are working with the most vulnerable people. Initially, this includes residents and workers in long-term care homes, frontline health-care workers, members of Indigenous communities, adult recipients of chronic home health care, adults 70 years of age and older and residents staying in shelters.
In Ottawa, more information about vaccines and who is eligible is available through the Ottawa Public Health website.
Why do some vaccines need two doses?
Some vaccines require two doses because the first dose may not stimulate the immune system enough to get a full response. The second dose will top your immunity up. In the case of the Pfizer COVID-19 vaccine, you get about 50 percent immunity with the first dose and 95 percent with the second dose.

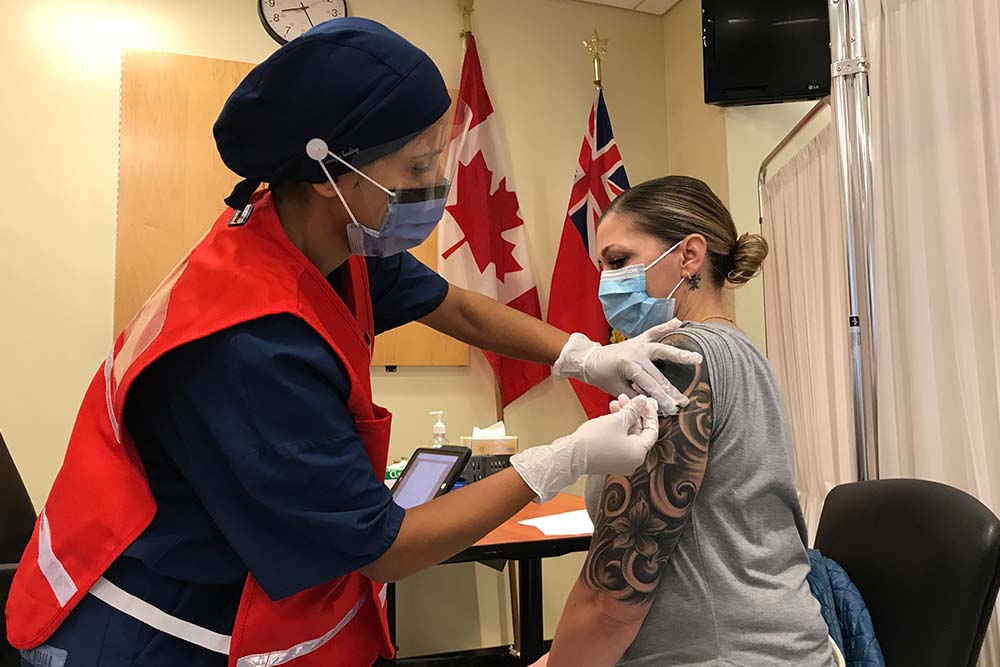
On Dec. 15, 2020, Jo-Anne Miner, a personal support worker at St. Patricks’ Home, was the first person to receive the initial dose of the Pfizer COVID-19 vaccine at The Ottawa Hospital’s Civic Campus. Jo-Anne received the second dose of the vaccine on Jan. 5, 2021.
What happens if a person doesn’t get the second dose of the COVID-19 vaccine?
The second dose of the COVID-19 vaccine is extremely important, and it can be a problem if you don’t get it because you won’t have maximum protection against the virus. In the case of the Pfizer COVID-19 vaccine, you may only have 50 percent protection with one dose. The second dose makes sure you have the highest level of immunity you can get.
Why has the interval between doses been extended in some scenarios? Will the vaccine still be effective if I get my second dose later?
Right now, the advice from NACI is that if vaccine supply is limited, jurisdictions should maximize the number of people who get their first dose by extending the interval for the second dose by up to four months. This is based on real-world data showing sustained protection after the first dose, as well as scientific principles.
NACI will continue to monitor the effectiveness of extended dose intervals and will adjust its recommendations as needed.
Will I get to decide which vaccine I get?
My recommendation, and the recommendation of experts around the world, is to get the first vaccine that’s offered to you. All Health Canada approved vaccines have strong efficacy protecting against severe illness. In the case of someone having a known allergy to one of the vaccine ingredients, they would be able to choose a vaccine that is safe for them.
More information about the efficacy of the vaccines approved by Health Canada is available on the Ottawa Public Health website.
If I’ve already had COVID-19, do I still need to get the vaccine? Or am I already immune?
We don’t know how well or how long someone can stay immune to COVID-19. The safest thing to do right now is to get the vaccine.
Does the vaccine still protect me against COVID-19 variants?
According to the World Health Organization, it’s likely that the vaccine will still protect you against COVID-19 variants. COVID-19 vaccines that are being developed or have been approved are expected to provide at least some protection against new virus variants because these vaccines elicit a broad immune response involving a range of antibodies and cells. This means that changes or mutations in the virus should not make vaccines completely ineffective. If any of these vaccines were found to be less effective against one or more variants, it’s possible to change the composition of the vaccines to protect against these variants.
However, the effectiveness of vaccines against COVID-19 variants will be monitored closely.
After getting the COVID-19 vaccine
Will I be able to stop wearing a mask and physical distancing after I get vaccinated?
People will still have to follow public health measures, like wearing a mask and physical distancing, after getting both doses of the COVID-19 vaccine because we still don’t know how truly effective the vaccine is in the real world and how long immunity lasts. We also aren’t certain if the vaccine prevents you from being infected with the virus while experiencing no symptoms, and still able to pass it on to others. Researchers around the world will be conducting studies to figure this out.
Communities will start to make decisions around changing public health measures only when they’re very confident that you have long lasting immunity, that the COVID-19 vaccine does prevent the transmission of the virus to other people, and that the vaccine is effective.
COVID-19 vaccine resources
Looking for more information about the COVID-19 vaccine? Check out these resources:
- COVID-19 vaccine – Ottawa Public Health
- COVID-19 vaccines for Ontario – Government of Ontario
- CANImmunize Inc. – a free digital tool for Canadians that securely stores your vaccination records and helps you get vaccinated on time. When eligible, the app will help you track your COVID-19 vaccinations and now includes standardized terminology and COVID-19 product information.
- What the COVID-19 vaccine does to your body – YouTube video by AsapSCIENCE
- Immunity Warriors: Invasion of the Alien Zombies – a digital comic to teach children about the immune system and the importance of immunization

Dr. Kumanan Wilson is a senior physician scientist in the Clinical Epidemiology Program and the Division of General Internal Medicine at The Ottawa Hospital. He is also professor in the Faculty of Medicine at the University of Ottawa, Innovation Advisor for Bruyere and founder and CEO of CANImmunize Inc.

Support patient care and research at
The Ottawa Hospital
You might also like…
Aging well: Guidance for older adults
In this special video series for both older adults and their loved ones, geriatric care specialists from The Ottawa Hospital offer guidance on navigating common health-care challenges that may arise with aging.
How to stay safe around water this summer
Drowning can happen to anyone — even strong swimmers. Emergency physician Dr. Christian Vaillancourt debunks common myths about drowning, explains how to act quickly to save a life, and shares what you can do to keep yourself and your loved ones safe around water.
What’s the difference between an optician, optometrist, orthoptist and ophthalmologist?
“Do I need to see an optician, optometrist, orthoptist or ophthalmologist?” We asked Ophthalmologist Dr. Annick Fournier to break down each role so you will know who to consult for your specific eye care needs.
Understanding rabies: Risks, vaccination and what to do after a bite
Although rare in Canada, rabies is almost always fatal once symptoms appear. Infectious diseases expert Dr. Michaeline McGuinty shares how rabies is spread, when to get vaccinated and what to do after a bite.
“My story doesn’t have to be your story”: New screening test better at preventing cervical cancer
“I went from being a 32-year-old new mom to a cancer patient with an incurable diagnosis.” Alicia’s journey underscores the critical role of HPV testing in preventing cervical cancer. Discover how the new HPV test can save lives and find out how to book your cervical screening appointment with our “Superscreener.”
Sign language interpretation services at The Ottawa Hospital: 5 FAQs
Do you require a sign language interpreter when you come to The Ottawa Hospital? For patients who are Deaf or hard of hearing, we provide both American Sign Language (ASL) and Langue des Signes Québécoise (LSQ) interpretation services at no cost. Before your next appointment with us, find out everything you need to know.


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.