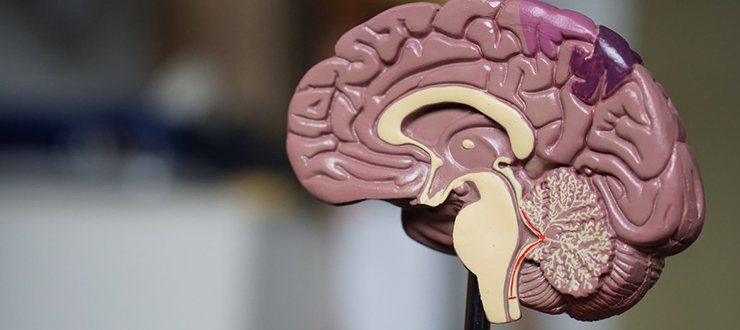
Although all human brains have the same general structure, the exact location of specific functions, such as speech, language comprehension even fine movements such as wiggling fingers, is slightly different in everyone. Small electrical impulses are put on the surface of the brain to help “map” it so that the neurosurgeon can try to avoid that area.
What is awake brain surgery?
Awake brain surgery, also known as an awake craniotomy, is a type of operation performed on the brain while the patient is alert and fully awake.
What kinds of patients might need awake brain surgery?
Awake brain surgery is used to treat patients who have certain types of brain tumors or lesions that may cause epileptic seizures. About 50 to 60 awake craniotomies are performed every year at The Ottawa Hospital, with most of them aiming to remove brain tumors that are located close to the part of the brain related to speech or movement. These parts of the brain are known as eloquent regions of the brain.
Does it hurt?
A specialized neuro anesthesiologist will give medications at the beginning of the surgery to make the patient sleepy and then give local anesthetic to ensure that the opening of the scalp and skull is relatively painless. Once the brain is exposed the patient is awoken.
Awake brain surgery is often a frightening prospect for every patient. The excellent team of surgeons, neuro anesthesiologists, nurses and allied health workers at The Ottawa Hospital deliver compassionate care to make each patient’s experience as easy as possible.
What does a patient experience during the awake brain surgery?

Once the patient is awake in the operating room, it’s time to “map” the brain. Everyone’s brain is a little different, so it’s important to know the exact location of different functions like language and movement of different parts of the body.
I would usually ask my patients to count backwards from 20, or to look at a picture of a simple everyday objects and say its name. As they do these tasks, I carefully apply a special electrode to a specific location on the surface of the brain. Then a small electrical current is put through the electrode for one to two seconds. This electrical current temporarily stops that particular part of the brain from functioning for that brief time.
I observe the patient carefully as I apply the electrode to different areas of the brain. If the patient suddenly stops speaking, then I suspect that the location of the electrode is also a part of the brain necessary for language.
I will further test this area of the brain to confirm that it is responsible for language. Then I know to avoid this area of the brain during my operation to remove the brain tumor. For more on mapping the brain’s language centres, read the story of Ron Wulf, a linguist who needed awake brain surgery to remove a brain tumour
I would ask my patients to lift up their hand and wiggle their fingers, as I use the electrode again to map which part of the brain is responsible for this action. When the patient stops wiggling their fingers or their hand drops on the bed then I am able to identify the motor centre of the brain responsible for hand movement. I do to same to map leg movements.
In this way I can map out certain functions of the brain in real time. By knowing which areas are important for speech and movement I avoid these areas as best as I can, while trying to take out all or most of the tumor.
How long does it take to go home after awake brain surgery?
In my practice, more than half of my patients who undergo an awake brain surgery will go home the very next morning. Some may have to stay a day or two longer in order to be monitored. My hope in the future is to be able to have the resources required to discharge the awake brain surgery patients on the same day of surgery. So, patients can have a brain tumor removed in the morning can have the afternoon tea in the comfort of their own home.

Support patient care and research at
The Ottawa Hospital
You might also like…
New radiation machine targets cancer with pinpoint accuracy — even as the tumour moves during treatment
“We can deliver a radiation treatment that’s exactly personalized for the patient on that day.” The Ottawa Hospital Cancer Centre is now one of the first in Canada to acquire the state-of-the-art MR-Linac radiation therapy system.
Watch: Princess Margriet of the Netherlands sent us this lovely video message for the Civic’s 100th anniversary
If you’ve ever wondered why tulips are so important to our city, the answer involves a world war, a royal family and The Ottawa Hospital’s Civic Campus. In this special video message, Her Royal Highness Princess Margriet of the Netherlands shares why the tulip is a special symbol of the endearing friendship between her country and Canada.
A volunteer program that taps into the power of music
Studies have shown that music can benefit the body, mind, relationships and community. Musical Moments is a program where volunteers play live music to support positive outcomes for patients, visitors and staff.
We’ve got you covered: The Ottawa Hospital now offers bandages for a variety of skin tones
Whenever you’ve scraped your knee or had your blood drawn, odds are your bandage was the same colour every time. Peach has been the default hue for over a century — but no longer at The Ottawa Hospital.
The Ottawa Hospital and YouTube Health partner to increase access to health information in Canada
Looking for health information online can lead you down a rabbit hole of misinformation. That’s why we’ve launched a series of videos with YouTube Health. Presented in both English and French by experts from across The Ottawa Hospital, these videos cover everything you need to know about an array of common medical conditions.
Looking to get screened for cancer but don’t have a family doctor? Make an appointment with our “Superscreener”
Regular cancer screening can help save lives. For people living in Eastern Ontario who do not have a primary care provider, the Champlain Screening Outreach Program offers screening services for breast, cervical, colorectal and lung cancer. Find out how to book your appointment with Nurse Practitioner Sarah Junkin-Hepworth, our “Superscreener.”


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.






Comment on this post