
Ashley Hilliard wants to share her story about having a miscarriage in the hopes it will help people know that support is available and they are not alone.
Miscarriage and pregnancy loss aren’t typical topics of conversation at dinner parties or on the front covers of magazines. But the reality is that one in ten pregnancies in Canada end in miscarriage. Ashley Hilliard, a 34-year-old recreation therapist living in Ottawa wants to shine a light on the topic of miscarriage by telling her own story.
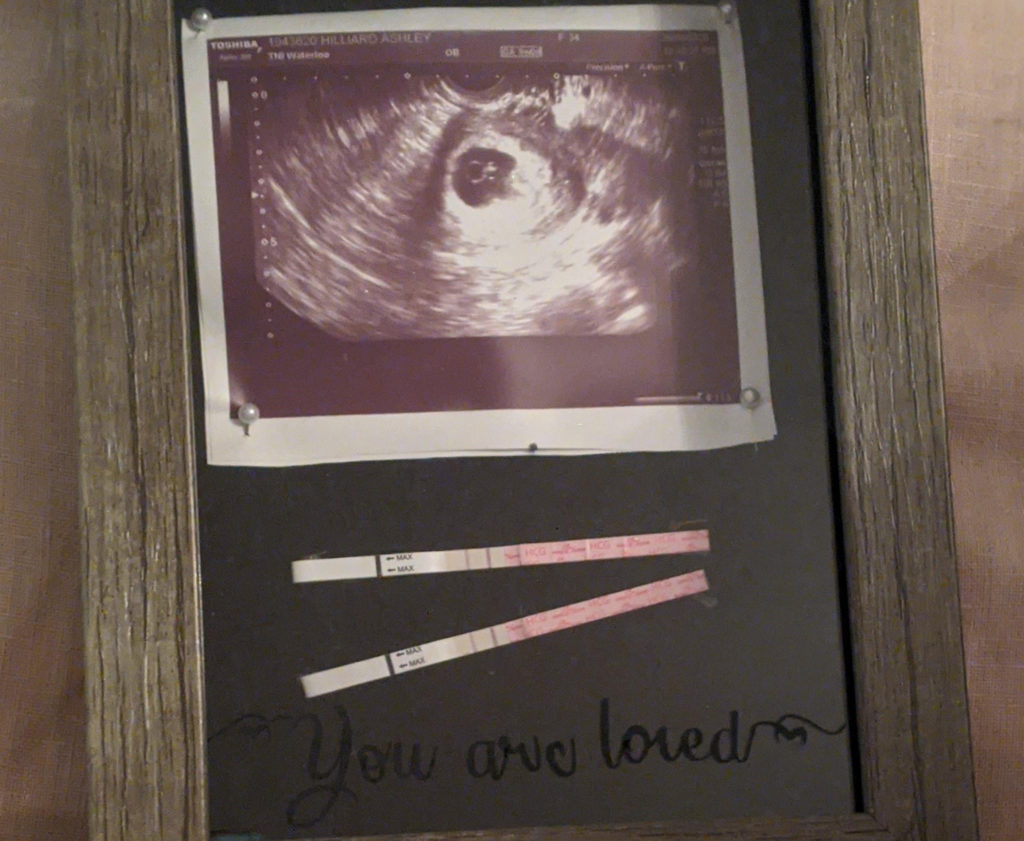
Ashley and her husband, Mike McDonald, were thrilled to discover Ashley was pregnant with their first child. They had been trying to conceive for the better part of a year before the positive test.
But her first ultrasound showed signs that the fetus was not growing as expected.
“We found out that our fetus was measuring quite small for where it should have been,” Ashley recalled. “It should have been about eight weeks, but it was measuring about six weeks, four days, so a significant gap. It also had a very slow heart rate, which was not a great sign.”
A follow-up ultrasound a few weeks later confirmed that the fetus didn’t have a heartbeat. The family was experiencing a miscarriage.
What is a miscarriage?
According to the Pregnancy and Infant Loss Network (PAIL), a miscarriage is the early delivery of a fetus, or the loss of a pregnancy before 20 weeks gestation. It is typically divided into two categories:
- early pregnancy loss: up to 12 weeks.
- late pregnancy loss: between 12 and 20 weeks.
Signs and symptoms of a miscarriage
According to Lindsey Davis, a registered nurse at the Family Planning and MVA programs at The Ottawa Hospital, the signs of miscarriage or pregnancy loss can include:
- bleeding from your vagina
- cramping in your lower abdomen, or
- no longer feeling other pregnancy symptoms such as breast tenderness or swelling.
If you experience any of these symptoms, call your health care provider.
Call 911 if you:
- bleed through one pad per hour for two hours, or
- feel cramping or pain so intense that it can not be managed.
Causes of a miscarriage
Many parents hope to find out the cause of their miscarriage or pregnancy loss. Sometimes the cause can be identified, but sometimes it can’t. Miscarriage is most often caused by a random error in the fetus’ chromosomes, which means the fetus cannot survive and the pregnancy ends. According to PAIL, other causes of pregnancy loss can include:
- infections
- hormone problems
- immune system responses
- medical conditions
- problems with the uterus or cervix
- problems with the placenta
it is common for people to feel responsible or a sense of guilt related to a miscarriage. It is important to know that, most of the time, a miscarriage is unpreventable. It does not happen because of something the pregnant person did wrong.
Kinds of miscarriage management
People who have a miscarriage typically have three options for how to manage it. Please talk with your health-care provider about which option might be right for you.
- Expectant: means waiting for the miscarriage to begin or end on its own without the use of medication or surgery.
- Medical: means taking medication that will help pass the pregnancy.
- Surgical: means having a surgical procedure in the hospital to remove the pregnancy tissue. A D&C procedure can be done at the Labour and Delivery Unit at the Civic or General campuses, or an MVA procedure can be done at the Riverside Campus.
Ashley’s choice
Ashley chose to take medication to help pass the pregnancy at home. She took the medication at 5 p.m. and went to bed later that evening.
“That’s when all hell broke loose,” she said.
“I woke up at 1:30 a.m. and could feel bleeding, which was expected,” she said. “I walked to the bathroom and had a mini hemorrhage. I asked my husband to get me clean pajamas, and when he came back I was unconscious.”
Mike called an ambulance because he couldn’t wake her up.
Ashley was rushed to the Emergency Department at the Civic Campus. There, the doctors stabilized her.
“I saw a really amazing doctor named Dr. Barb Miller. She and others monitored me and took really good care of me. I felt much better and was able to go home.”
Ashley felt cramping a few days later and Mike drove her back to the Emergency Department.
“Both times through the Emergency Room, I had top-notch care,” she said. “They were very respectful, very dignified. I was super impressed with how everybody treated what could be seen as a delicate situation. I saw another great doctor named Dr. Justine Amaro who referred me to the Early Pregnancy Evaluation Clinic at The Ottawa Hospital. That was Sunday. Monday morning, the clinic called me with an appointment for the next day.”
About the Early Pregnancy Evaluation Clinic
The Early Pregnancy Evaluation Clinic at The Ottawa Hospital works closely with the Emergency Department to provide care to patients who arrive in the early stages of their pregnancy. Those who are referred to the Early Pregnancy Evaluation Clinic typically receive an appointment at the clinic within one or two days. This means they have a shorter wait in the Emergency Department and can typically rest at home.
“I have 750 friends on Facebook, and guaranteed somebody on there has gone through this.”
The clinic acts like a hub. From there, patients can be referred to a variety of professionals, including an OB/GYN to have an ultrasound and to make a plan of how to proceed.
Ashley appreciated how well the Early Pregnancy Evaluation Clinic worked for her.
“Being part of the Early Pregnancy Evaluation Clinic gave me a contact person,” she said. “I knew this is what they do and this is what they manage. I didn’t have to go through the Emergency Department every time. I’m glad I had that continuity of care.”

If a pregnancy loss is confirmed, patients who choose to manage it surgically can have a D&C procedure done at the Labour and Delivery Unit at either the General Campus or Civic Campus. However, many patients who have a miscarriage prefer not to receive care next to parents who have recently given birth to full-term babies, and opt for the MVA clinic instead.
The MVA program was introduced at the Shirley E. Greenberg Women’s Health Centre at the Riverside Campus by Davis, Dr. Pamela Berger, Dr. Amanda Black. The program was created specifically to meet the needs of parents and partners who have experienced a pregnancy loss and is the first of its kind in Canada.
“I often tell people that this is a safe place for you to feel whatever it is you need to feel,” said Davis. “Sometimes patients have held it together for their partner or their other children or their families and once they get to the program, they fall apart a little bit, and that’s ok. For other people, this is the last stop. They have all the support they need. Their partners are wonderful, their families are wonderful, the shape of this pregnancy loss has changed for them and they are ready to have the procedure.”
There is no “right” way to feel after a miscarriage
Davis has years of experience supporting patients, partners and families who have experienced pregnancy loss. She knows that there is no such thing as a typical reaction to a miscarriage.
“Everyone is different, and no reaction is wrong,” she said. “No response, no feeling, no way of understanding what they are experiencing is wrong. Whatever they are experiencing is their truth, and certainly we want to support that.”
Davis has seen a range of reactions – from extremely emotional to stoic. Some patients don’t know how to feel.
“Some people say ‘is that bad? Is it bad that I’m not crying? Should I be crying?’ and we tell people that it’s ok to feel however they feel. There is no right way to be.”
For Ashley, the physical toll her body has taken has been more intense than the emotional one.
“I totally understand that different people handle this in different ways,” she said. “It could be years later and people are still having an emotional response. For me, it was more the physical stuff.”
Ashley’s story continues
Ashley says that she and Mike are doing well, and is grateful for the care she received at The Ottawa Hospital.
Thousands of families across Canada have their own miscarriage stories – some will be similar to Ashley’s and some will be very different. Ashley hopes that by telling her story, she can help people understand that they are not alone.
“I have 750 friends on Facebook, and guaranteed somebody on there has gone through this,” she said. “But it’s such a taboo subject, and it seems to be such a secret. Now I think, ‘how can I improve this for other people?’ I think we handled it well, but not everybody does.”

Support patient care and research at
The Ottawa Hospital
You might also like…
Ask Masi: A new support tool for front-line perinatal care providers
Parents will often describe welcoming a new child as one of the happiest times of their lives. But physicians, midwives, nurses and others on the front lines will tell you that this is not always the case for their patients. A new service for care providers called Ask Masi is here to help.
Watch: Princess Margriet of the Netherlands sent us this lovely video message for the Civic’s 100th anniversary
If you’ve ever wondered why tulips are so important to our city, the answer involves a world war, a royal family and The Ottawa Hospital’s Civic Campus. In this special video message, Her Royal Highness Princess Margriet of the Netherlands shares why the tulip is a special symbol of the endearing friendship between her country and Canada.
A volunteer program that taps into the power of music
Studies have shown that music can benefit the body, mind, relationships and community. Musical Moments is a program where volunteers play live music to support positive outcomes for patients, visitors and staff.
We’ve got you covered: The Ottawa Hospital now offers bandages for a variety of skin tones
Whenever you’ve scraped your knee or had your blood drawn, odds are your bandage was the same colour every time. Peach has been the default hue for over a century — but no longer at The Ottawa Hospital.
Patient gifts a piece of home to Indigenous Cancer Program
Inuit patients can now see and hold a piece of their traditional territory in the Windòcàge Room at the General Campus, thanks to an interactive gift donated to The Ottawa Hospital by a cancer patient.
Second Chance: Don’s song for the people who saved his life
Making music has always been a big part of Don’s life, so when the staff and doctors at The Ottawa Hospital saved him from the brink of death, he could think of no better way to thank them.


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.






Comment on this post