
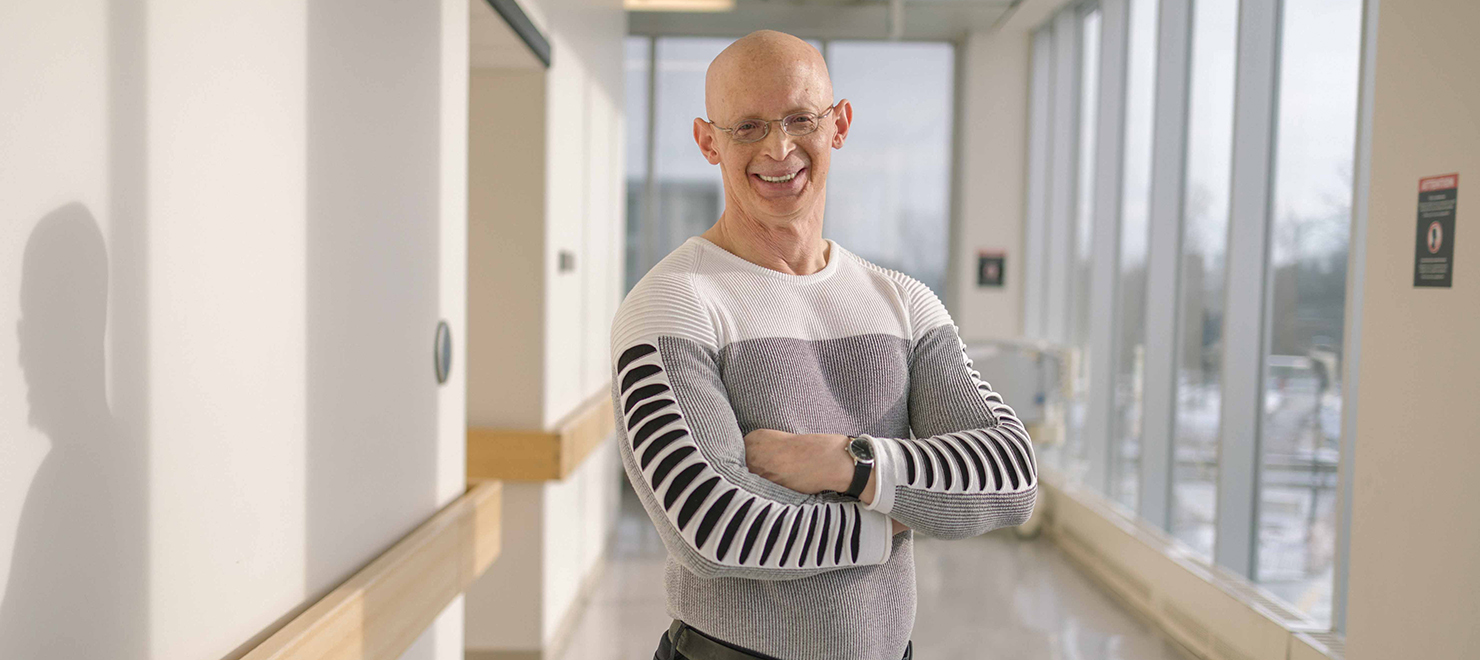
Dr. Andrew Seely developed the innovative device, which he believes will help improve patient care.
The Ottawa Hospital is the first hospital in the world to evaluate an innovative medical device that uses artificial intelligence (AI) to predict when critically ill patients are ready to breathe on their own, called the Extubation Advisor. The device was developed by Dr. Andrew Seely, a critical care physician, thoracic surgeon and scientist at The Ottawa Hospital and founder and CEO of Therapeutic Monitoring Systems (TMS).
A medical first
Over the last two years of the pandemic, more Canadians than ever have experienced extreme difficulty breathing, requiring mechanical ventilation (intubation) in critical care units across the country. According to the Ontario Science Table, at the peak of wave three, the number of patients on ventilators was more than 180 percent of pre-pandemic historical averages, and the recovery is not easy.
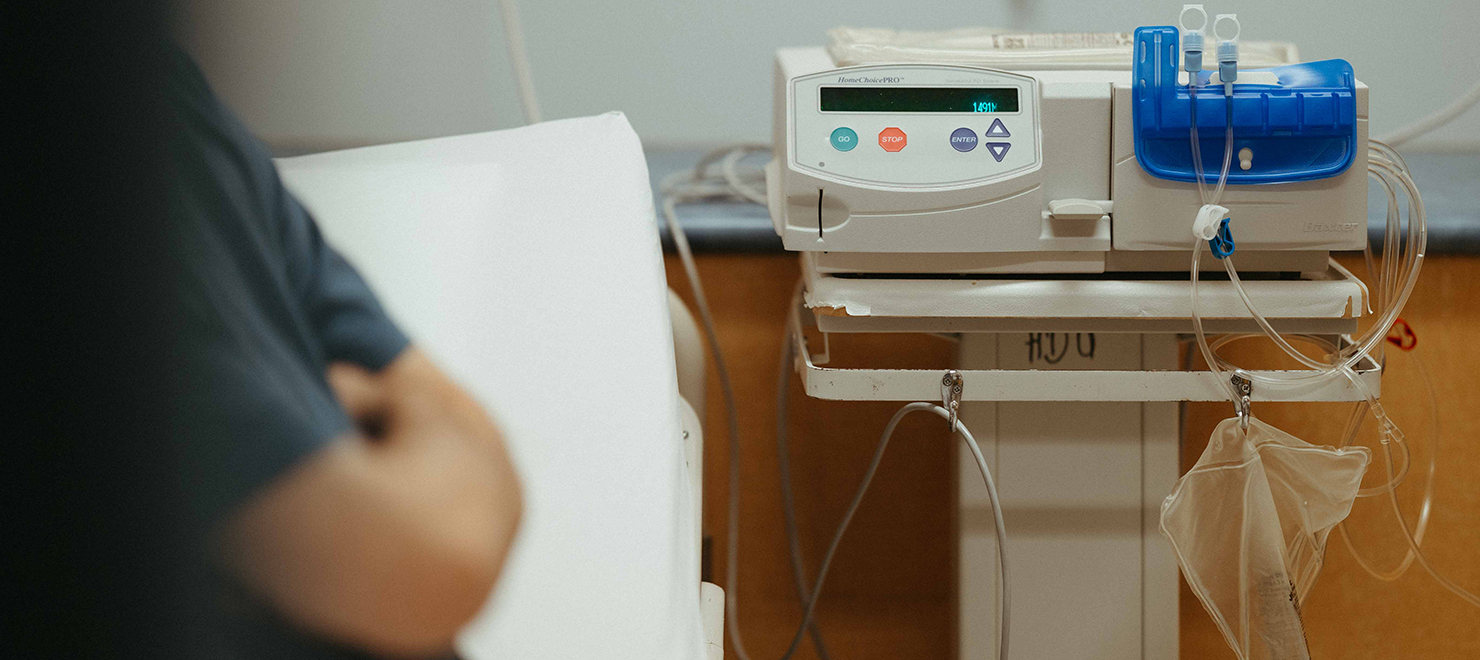
A mechanical ventilator is a machine that helps patients breathe when they cannot breathe on their own due to critical illness, such as COVID-19, or surgery. The machine is connected to a breathing tube that is inserted into the patient’s trachea. The process of intubating (inserting the tube) and extubating (removing the tube) is very complex, and anyone requiring ventilation will require months of recovery and rehabilitation to learn how to swallow, eat, talk and breathe again. Currently, there is no patient monitoring equipment to help physicians decide the best time to remove a patient from a ventilator to improve their outcomes, but Dr. Seely and his team are well on their way to changing that.

Over the last 13 years, Dr. Seely and his colleagues have made major progress in using complex mathematics, artificial intelligence and routinely collected vital sign data to predict when patients are ready to be extubated. Dr. Seely founded TMS in 2007 to further develop the research and bring it closer to helping patients. In 2019, TMS partnered with manufacturer OBS Medical to bring their design and concept to life, and this year, the system was used for three months at the bedside of ventilated patients in The Ottawa Hospital’s Intensive Care Unit (ICU), with permission from their families.
A step in the right direction

“Currently, one in every seven ICU patients experiences extubation failure. Prolonged ventilation harms patients, and early extubation requiring reintubation can be a devastating blow to their recovery,” says Dr. Seely, who is also a professor at the University of Ottawa. “We’ve developed the first medical device to offer extubation decision support, which we believe will help standardize and improve care.”
The device constantly monitors and analyzes a patient’s vital signs, including blood pressure, oxygen levels, breathing rhythms and heart rate during their ventilation. Then, it uses AI to provide doctors with a specific read of when the patient can be safely removed from the ventilator. This is the first time that real-time predictive analytics based on this type of high-frequency data is being used and evaluated at the bedside.
Dr. Seely and his team hope this tool will help improve patient safety and outcomes in the near future. After the successful three-month initial evaluation at The Ottawa Hospital, the metrics are looking promising, and the feedback received from physicians was very positive.
“What Dr. Seely and TMS are doing is revolutionary. It’s the future of medicine,” says Dr. Kwadwo Kyeremanteng, Department Head of Critical Care at The Ottawa Hospital. “This kind of technology will allow us to make more informed decisions that are precise and patient centered. This will allow for better outcomes and improved resource use. Honestly, this is groundbreaking research.”
Dr. Seely and his team’s next steps include a randomized controlled trial. With each milestone, they are one step closer to transforming care for some of the sickest patients treated at hospitals.
“Although there is still work to be done to evaluate clinical impact, this first-time bedside implementation is a step in the right direction of transforming routine monitoring into improved care,” says Dr. Seely. “We are grateful to our partners, collaborators, consenting patients and research team who are enabling this innovation.”
All researchers at The Ottawa Hospital follow a Responsible Innovation framework for developing and commercializing innovations in a responsible way.

Support patient care and research at
The Ottawa Hospital
You might also like…
New gender-affirming surgery clinic now accepting patients
The Ottawa Hospital’s new gender-affirming surgery clinic is truly one of a kind. Launched in September 2023, it’s the only clinic in Ontario to offer trans and non-binary patients facial, top and bottom procedures. Plastic Surgeon Dr. Nicholas Cormier and his team are happy to announce that they are now accepting patient referrals from physicians.
Mental health professionals and paramedics team up to help people in crisis
Seven days a week, a mental health professional from The Ottawa Hospital hits the road with a paramedic from the Ottawa Paramedic Service. Together, they respond to 911 calls for mental health emergencies across the city. Social worker Cindy Gill and paramedic Scott Farrell share how the Mental Wellbeing Response Team provides quality care for patients out in the community.
“Stewards of hormones”: Our Gender Diversity Specialty Clinic guides medically complex patients on their affirmation journey
Often, trans and non-binary patients struggle to find health-care providers to support them on their affirmation journey. It is even more difficult for patients with complex medical needs. That’s why we launched our Gender Diversity Specialty Clinic, one of the first of its kind in Canada.
The comfort of home: Home Dialysis Program empowers patients to live more independent lives
For people living with kidney failure, the most ideal form of dialysis treatment is done in the place where they are most comfortable—their home. Five years ago, we transformed our Home Dialysis Program, enhancing quality of life for our patients, welcoming more patients, and turning it into a model for dialysis programs across the province.
New Research Chair in Gay Men’s Health is setting out to break down barriers to care
As both a researcher and a gay man, Dr. Paul MacPherson knows all too well the stigma that gay men often face in the health-care system. Now, as the Clinical Research Chair in Gay Men’s Health at The Ottawa Hospital and the University of Ottawa, he’s on a mission to make quality health care more accessible to this often overlooked patient population.
The Ottawa Hospital administers world-first in-utero treatment for rare genetic disorder
Before Ayla was born, she had already made history. Last year at The Ottawa Hospital, she received a world-first in-utero treatment for Pompe disease, a rare genetic disorder that had taken the lives of two of her siblings. Now 17 months old, Ayla is healthy and happy.


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.




Comment on this post