France Todd (centre) was part of a pilot study to reduce the amount of blood patients lose during liver surgery and limit their need for blood transfusions.
France Todd’s liver cancer came out of the blue.
“It was one of those flukes,” said the avid downhill skier, CrossFitter, and mother of two. “I went in for my annual check-up and my family doctor found traces of blood in my urine.”
Suspicious spots on an MRI and a biopsy confirmed that she had a tumour.
“My surgeon, Dr. Guillaume Martel, recommended having it removed the following week,” said Todd, who was the director of human resources of a high-tech company at the time. “I was in shock. I knew it would be a big disruption to my life.”
Thankfully, surgery to remove the 4-centimetre tumour went smoothly. Todd did not need a blood transfusion, unlike 25 percent of patients who undergo liver surgery.
Todd was part of a pilot study to test whether taking out 10 percent of a patient’s blood before liver surgery, about the same volume as a blood donation, would reduce their bleeding during the operation.
“We basically removed blood from the patient into a blood donation bag before the surgery, and then put it back in once surgery is done,” said Dr. Martel, a surgeon at The Ottawa Hospital and associate professor at the University of Ottawa. “This technique has been around for a long time. People feel intuitively that it works, but it’s never been rigorously tested.”
The technique is now being investigated in clinical trials, as part of Dr. Martel’s larger research program to reduce unnecessary blood transfusions during liver surgery.
He and his colleagues have also published a tool to help liver surgeons decide when blood transfusions are appropriate. The criteria, based on the latest research and expert opinions, will need to be validated in the clinic.
“Transfusions on one hand are life-saving,” said Dr. Martel. “But on the other hand there are some small risks associated with them, such as infections, allergic reactions, cardiovascular effects and possibly worse cancer results after surgery. We should really be trying to avoid blood transfusions unless they’re absolutely necessary.”
This research was possible because of generous support for The Ottawa Hospital in research to improve patient care. These studies were also supported by the Canadian Surgical Research Fund and the Department of Surgery at the University of Ottawa.

Support patient care and research at
The Ottawa Hospital
You might also like…
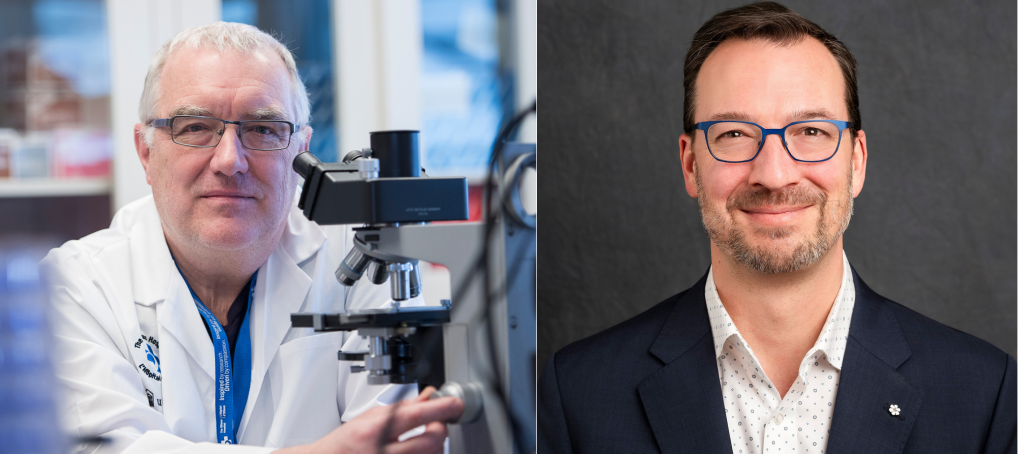
Dr. John Bell and Stephen Beckta inducted into the Order of Canada
The Ottawa Hospital is proud to share that on December 31, 2025, two members of our team were inducted into the Order of Canada. Congratulations Dr. John Bell and Stephen Beckta.
Everyone at our hospital plays a role in research. Here’s how
It’s Research Week at The Ottawa Hospital. Check out this video to hear from some of the incredible people fuelling our discoveries that are having an impact around the world.
New program fills gap in care for teens and young adults with cancer
For young people, a cancer diagnosis can disrupt their education, careers, relationships and family-building goals. Our Adolescent and Young Adult (AYA) Cancer Program supports AYAs on their cancer journey, complementing the care provided by their care team.
Do you have a surgery coming up? Here are five “prehab” tips to help you recover faster
You’ve probably heard about rehabilitation, but what about “prehabilitation”? Prehab is all about getting your body and mind in top shape before surgery so you can enjoy a smoother, quicker recovery. Discover five essential prehab strategies from researcher Dr. Daniel McIsaac.
“My story doesn’t have to be your story”: New screening test better at preventing cervical cancer
“I went from being a 32-year-old new mom to a cancer patient with an incurable diagnosis.” Alicia’s journey underscores the critical role of HPV testing in preventing cervical cancer. Discover how the new HPV test can save lives and find out how to book your cervical screening appointment with our “Superscreener.”
By thinking differently, this research team is improving the lives of people with cancer
Taking a different approach to clinical trials, the REthinking Clinical Trials (REaCT) program aims to answer some of the most important and practical questions that affect both patients with cancer and our health-care system. Find out what sets REaCT apart and makes the program so special to participants like Beth.


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.