How do I quit smoking?
I’ve smoked my whole life. How can I stop?
Do quit smoking products and programs really work?
If you have ever asked yourself these questions, you’re not alone. Emilie Serano, an advanced practice nurse in the Smoking Cessation Program at the University of Ottawa Heart Institute, hears them from people every day. More and more Canadians are reaching out for help to quit smoking.
Despite how daunting it might feel, especially amidst the stress of a pandemic, quitting for good is possible. The Ottawa Hospital has supportive, evidence-based stop smoking programs to help you.
Read Emilie’s answers to FAQs about quitting smoking.
The health hazards of smoking are well documented, and if you’re a smoker, you’re likely well-aware of them. According to Health Canada, “There is strong medical evidence that smoking tobacco is related to more than two dozen diseases and conditions. It has negative effects on nearly every organ of the body and reduces overall health. Smoking tobacco remains the leading cause of preventable death and has negative health impacts on people of all ages: unborn babies, infants, children, adolescents, adults, and seniors.”
So, if smoking is so unhealthy, why do people do it?
Stressful times (like a pandemic) can trigger unhealthy behaviours
Although smoking has been an important health topic for decades, it is especially significant during the COVID-19 pandemic. Research directly linking smoking rates to the COVID-19 pandemic are still underway, but a synopsis from Public Health Ontario suggests that the conditions are ripe for an increase in smoking rates.
“Although we did not identify studies addressing smoking and relapse from abstinence during an epidemic, previous studies have suggested that people who smoke and are exposed to natural disasters tend to smoke more than those unexposed and that people with past smoking are more likely to relapse. Activities such as smoking and other substance use could increase, not only as a form of distraction or behavioural avoidance strategy, but also as a result of the stress, anxiety or depressive symptoms that many are experiencing during the COVID-19 pandemic. There is also concern that these changes could lead to relapse from abstinence.”
In other words, we know that people who experience a stressful event may try to cope with it by starting smoking (if they had quit in the past) or smoking more (if they currently smoke). And for many of us, the pandemic has been very stressful.
Don’t be deceived: Smoking doesn’t lower stress—it fuels it
“Smoking increases your heart rate, your blood pressure, and your fight-or-flight response,” said Emilie. “What you’re actually reacting to when you light a cigarette is not stress, but a craving caused by stress. What your body really wants is more dopamine. When you give your brain the dopamine, you feel relieved – so it creates a false impression that smoking actually helps with stress.”

So what can you do if you want to quit smoking but aren’t sure how? The Ottawa Hospital has several smoking cessation programs to help patients in the hospital and people in the Ottawa area.
Smoking cessation programs at The Ottawa Hospital
The Ottawa Model for Smoking Cessation
The Ottawa Model for Smoking Cessation is an evidence-based process to help people who are receiving care in the hospital quit smoking. The program was developed by the University of Ottawa Heart Institute and is used at hospitals across Ontario.
The Quit Smoking Program
The Quit Smoking Program at The University of Ottawa Heart Institute is led by a nurse who specializes in smoking cessation who will give you one-on-one support through your journey. Together, you will make a personalized “quit plan,” which may include medication. Follow up appointments are scheduled monthly for six months. You can refer yourself to the program, or ask your doctor to refer you.

Support patient care and research at
The Ottawa Hospital
You might also like…
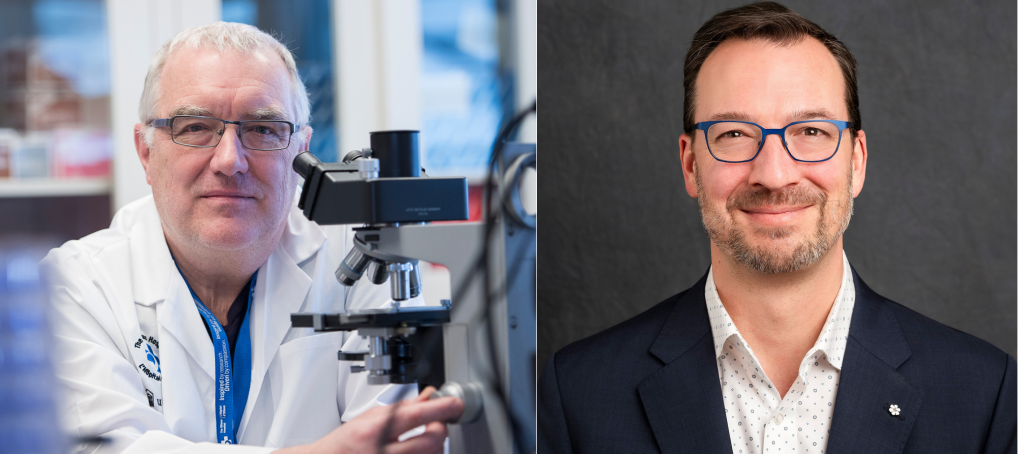
Dr. John Bell and Stephen Beckta inducted into the Order of Canada
The Ottawa Hospital is proud to share that on December 31, 2025, two members of our team were inducted into the Order of Canada. Congratulations Dr. John Bell and Stephen Beckta.
Living with chronic pain? This online tool offers help — and hope
The Power Over Pain Portal is a free virtual resource hub designed to help empower youth and adults living with chronic pain through education and peer support.
What to do in an emergency: New first aid video series on YouTube
Would you know what to do if you saw someone experience a stroke, heart attack or opioid overdose? We’ve launched a series of easy-to-follow videos on YouTube that walk you through how to respond to common first aid emergencies.
Flu season 101: A quick guide to keeping the sniffles away
Got two minutes? This short guide could help you make it through flu season without stocking up on tissues.
New program fills gap in care for teens and young adults with cancer
For young people, a cancer diagnosis can disrupt their education, careers, relationships and family-building goals. Our Adolescent and Young Adult (AYA) Cancer Program supports AYAs on their cancer journey, complementing the care provided by their care team.
Celebrating the summer solstice and National Indigenous Peoples Day: A photo essay
The summer solstice has deep spiritual and cultural significance for Indigenous communities around the world. Last week, we joined CHEO and uOttawa for a special celebration to mark this important time of year, and to recognize the rich cultures of First Nation, Inuit and Métis Peoples.


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.