
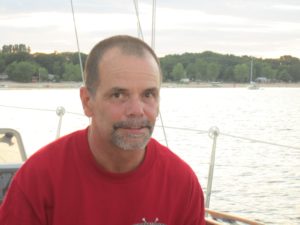
Sailing enthusiast Peter Juryn joined a pilot study that put him in charge of managing his Parkinson’s disease. An expert nurse helped him set his own care priorities and referred him to health-care professionals who specialize in his care needs.

Sailing is a life-long love affair for Peter Juryn that began when was nine years old. He now sails out of the Nepean Sailing Club, where he also helps out with the boats and hangs out with his friends.
Unfortunately, the medication he takes for Parkinson’s disease was keeping him awake for hours during the night, making it harder to do the things he loves.
During an appointment, Dr. Tiago Mestre and nurse Diane Côté asked if he would like to take part in a study looking at a new way of delivering Parkinson’s care.
“I said ‘Sure, I’ll help. What can I do?’” said Juryn. “I’d like to help the system work better. If it can help me as well, then that’s great too.”
Juryn was paired with Côté, a specialized Parkinson’s nurse, who helped him identify his three care priorities: sleep, speech and exercise.
“I’m more in the driver’s seat,” said Juryn, who has lived with Parkinson’s disease since 2001. “I’m kind of building more of a team around me, based on these priorities.”
Juryn is currently treated with deep brain stimulation for his Parkinson’s, which reduced his medication and improved his sleep. But simple tips like moving his desk and computer out of his bedroom also made a difference.
“I built a sleep sanctuary of sorts, free from all blue screens,” said Juryn.
Côté also lined up a referral to a sleep clinic and to a speech therapist, all without Juryn having to see a neurologist. Thanks to a care network created by the researchers, she was able to direct him to professionals with knowledge of Parkinson’s disease. Peter has joined a specialized speech therapy program for people with Parkinson’s, and his voice and swallowing have already improved. He also joined a gym where he exercises three to four times a week.
“There’s a lot of demand for Parkinson’s neurologists, and patients often wait months between appointments,” said Côté. “By referring patients to specialized caregivers in the community, we can improve their quality of life with little cost to the system.”
Dr. Mestre received a $197,000 New Investigator Award to test this new model of care, called the Integrated Parkinson’s Care Network, which was developed in collaboration with Dr. David Grimes. The pilot study at The Ottawa Hospital has recruited almost all the 100 patients it needs after only four months. If it is successful, the model may be introduced to other sites across Ontario and Canada.
“I’m excited about this project because it has the potential to make a real difference for our patients, and the results are immediate,” said Dr. Mestre, a Parkinson’s neurologist at The Ottawa Hospital and an assistant professor at the University of Ottawa Brain and Mind Research Institute. “We believe that this patient-centred model can improve quality of life for the 100,000 Canadians living with Parkinson’s disease.”
Juryn has been very satisfied with the care he’s received.
“All the staff are really helpful, and they obviously care,” said Juryn.
“I am very proud of Peter for his accomplishments and the things he is doing to improve his quality of life since entering the study,” said Côté.
This research is also supported by generous donations to The Ottawa Hospital and the University of Ottawa Brain and Mind Research Institute.

Support patient care and research at
The Ottawa Hospital
You might also like…
From survivor to supporter: Peer volunteers bring hope to patients recovering from stroke
Drawing on their own lived experiences as stroke survivors or caregivers, volunteers with March of Dimes Canada’s After Stroke Hospital Peer Connections program offer emotional support to those just beginning their recovery journey. Discover the difference they’re making and learn about how you can request support for a loved one — or become a beacon of hope yourself.
Sign language interpretation services at The Ottawa Hospital: 5 FAQs
Do you require a sign language interpreter when you come to The Ottawa Hospital? For patients who are Deaf or hard of hearing, we provide both American Sign Language (ASL) and Langue des Signes Québécoise (LSQ) interpretation services at no cost. Before your next appointment with us, find out everything you need to know.
The place to be: The Ottawa Hospital recognized as one of Canada’s most admired corporate cultures
The Ottawa Hospital (TOH) has been named one of Canada’s most admired corporate cultures. Guided by compassion and commitment to patient care, TOH has developed a workplace culture that inspires confidence and trust in our employees, patients and family members.
Watch: Princess Margriet of the Netherlands sent us this lovely video message for the Civic’s 100th anniversary
If you’ve ever wondered why tulips are so important to our city, the answer involves a world war, a royal family and The Ottawa Hospital’s Civic Campus. In this special video message, Her Royal Highness Princess Margriet of the Netherlands shares why the tulip is a special symbol of the endearing friendship between her country and Canada.
A volunteer program that taps into the power of music
Studies have shown that music can benefit the body, mind, relationships and community. Musical Moments is a program where volunteers play live music to support positive outcomes for patients, visitors and staff.
We’ve got you covered: The Ottawa Hospital now offers bandages for a variety of skin tones
Whenever you’ve scraped your knee or had your blood drawn, odds are your bandage was the same colour every time. Peach has been the default hue for over a century — but no longer at The Ottawa Hospital.


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.





