toh
General X-Ray

What is an X-Ray (Radiography)
“X-ray” or radiography is a type of diagnostic imaging modality that uses a very small amount of X-ray radiation to produce pictures of the body’s internal structures.
X-rays are the oldest and most frequently used form of medical imaging.
They are often used to help diagnose lung and abdominal diseases, fractured bones, injured joints and even to study blood vessels and locate foreign objects in soft tissues, among other applications.
For some specific x-ray exams, an iodine-based or barium contrast material is used to help improve the visibility of the organs or blood vessels.
Who performs the exam?
A highly trained Medical Radiation Imaging Technologist (MRIT) will perform your X-Ray.
The MRIT will consult with the Radiologist (the physician specialized in medical imaging) if there any questions or concerns regarding your X-ray study.
What does having an X-Ray feel like?
An x-ray examination is painless.
At times, though, you might experience a small amount of discomfort from the cool temperature in the examination room or the hardness of the X-ray table. Also, you may find that the positions you need to hold might be uncomfortable or painful, especially if you have an injury.
Our specialized technologists will assist you in finding the most comfortable position possible to make sure we get the best possible pictures need for diagnosis.
Safety information
You should inform your technologist if there is a possibility of being pregnant, if you are using an insulin pump or have a known allergy to iodinated contrast media (“X-ray dye”).
You should also inform your technologist if you have problems standing or need any assistance.
What are the Risks of X-Rays?
- There is no strong statistical evidence to prove that the low levels of radiation used in diagnostic imaging has any negative effects on your health. However, The Ottawa Hospitals’ view is to assume all radiation exposure might impose some risk.
- The Ottawa Hospital abides by the principle known as “ALARA” (As Low As Reasonably Achievable), which means we keep radiation doses as low as possible, without compromising the image quality of your study.
- The amount of radiation exposure varies from one procedure type to another, and different parts of the body present different sensitivity to it.
- During some X-ray studies, you might be asked to wear a lead apron or use a lead shield over specific areas, which will shield the other parts of your body (not being imaged) from radiation.
Is Radiation only originated by X-rays?
No, natural radiation exposure comes from the earth in rocks and soil and from outer space, in the form of cosmic rays. A small amount of radioactive material even exists naturally in our bodies.
Every year, each person is exposed to this natural radiation and radiation from a variety of other sources, including household smoke detectors, fertilizers and certain foods. Air travel also increases exposure to cosmic radiation due to the higher altitudes and less atmospheric shielding.
Naturally occurring background radiation and modern activities such flying in an airplane all contribute to a lifetime exposure, which is only slightly increased by medical imaging.
How does X-ray radiation create an image?
X-ray radiation is a type of electromagnetic wave with very high frequency, with many properties in common with light, radio waves and other forms of electromagnetic waves.
rays are generated by a special component in the machine (the “tube”). They have enough energy to pass through the The various tissues in the body absorb X-ray radiation differently and the radiation then reaches a detector on the other side of the machine, in which the image is created. The image corresponds to the X-ray “shadow” of the area that was exposed.
The study is then sent into a specific computer system of the hospital that allows it to be reported and be part of your medical chart.
What happens after my examination?
Once the study is ready to the reported, a Radiologist, a specially trained physician for diagnosis and procedures using medical imaging, will interpret the images and generate a document, called a report.
The report will then be available to the responsible medical team. A radiologist is also always available at any time at The Ottawa Hospital, so that your doctor can get an answer to specific doubts regarding the study or the report.
The valuable information gained from the X-ray examination allows your doctor to take important decisions about your health.
Exams performed at TOH
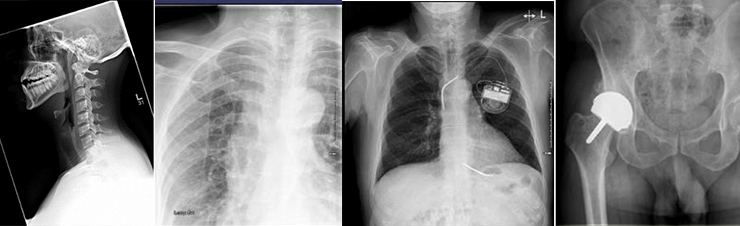
Many examinations can be performed with X-Rays.
They include conventional studies such as Chest, Abdominal, Joints and extremities radiographs, among may variants.
Special studies and imaging-guided procedures can also be done with the use of X-rays. Most are done with the use of a Fluoroscopy machine, a type of X-ray machine that allows real time low dose imaging, including the ability to create continuous imaging (cine clips) and dynamic assessment of structures/contrast media motion.
Some of these are detailed below. They are always performed by a Radiologist or other specialized physician, assisted by the Medical Radiation Imaging Technologist, at times with nurses and additional staff.
Special procedures: Musculoskeletal system
Arthrograms/joint injections: A minimally invasive procedure to obtain images of joints with the use of a minimal amount of contrast media. Usually, this is performed in conjunction with a joint injection, for treatment of pain.
Aspirations/Biopsies: A minimally invasive procedure whereby a sterile needle and syringe are used to collect fluid/tissue from a patient’s joint, bone or soft tissues.
Special procedures: Spine
Lumbar Puncture: A minimally invasive procedure in which a thin needle is inserted into the lower part of the spine to test for conditions affecting the brain, spinal cord or other parts of the nervous system. You will be required to remain in the department for a short amount of time after the procedure is complete to recover.
- Diagnostic Lumbar Puncture: During the procedure, pressure can be measured and samples of cerebrospinal fluid (CSF) are collected and sent for testing.
- Myelogram: Contrast media is injected into the spinal canal to identify problems of the spinal cord, nerve roots, and other tissues. You may be asked to have a CT scan after the procedure.
- Nuclear Medicine Cisternogram: Radioactive liquid is injected into the spinal canal to determine if there are changes to the cerebral spinal fluid (CSF) flow within the brain and spinal canal.
- MRI/CT Cisternogram: contrast media is injected into the spinal canal to diagnose spinal fluid leaks using Computed Tomography (CT) and/or Magnetic Resonance (MRI).
- Chemotherapy injection: samples of cerebrospinal fluid (CSF) are collected and sent for testing. A cancer treatment medication is then injected into the spinal canal for the treatment of different types of cancers.
Special procedures: Gastrointestinal studies
Gastrointestinal Studies are examinations of the gastrointestinal (GI) tract using barium or water-soluble contrast media.
- An upper gastrointestinal series (UGI) is an X-Ray exam of the upper gastrointestinal (GI) tract, corresponding to the esophagus, stomach, and duodenum (first part of the small intestine). You will be given the contrast with gas granules to swallow during the procedure.
- A barium enema is an X-ray exam that can detect changes or abnormalities in the large intestine (colon). An enema is the injection of a liquid into your rectum or into a surgical opening in the abdominal wall through a small tube.
- A proctogram is an X-ray exam that is used to investigate patients who have problems emptying their bowels and have symptoms of obstructed defecation. The test shows how well the bowel empties.
- A Colonic Transit Study is an X-ray exam performed to monitor to passage stomach contents through the entire digestive tract. You will be provided a pill to ingest that contains markers that are visible on X-ray 5 days before you come for the exam.
Feeding Tube Insertion/Check
- Insertion: The Radiologist will insert a feeding tube gently down your throat while you’re lying down. You may also be asked to bend your head, neck, and body at various angles as they thread the tube through your nostril, down your esophagus, and into your stomach. These movements can help ease the tube into position, without causing you too much pain or discomfort. They may also ask you to swallow or take small sips of water when the tube reaches your esophagus to help it slide into your stomach.
- Check: Once your feeding tube is in place, the Radiologist will check its placement by injecting contrast into the tube. To keep your feeding tube in place, the Radiologist will likely secure it to your face with a piece of tape. They can reposition it if it feels uncomfortable.
Cholangiography
Cholangiography an examination of the bile ducts, also known as the biliary tree.
- Contrast media is injected through the T-shaped tube left in the common bile duct. Imaging of the biliary tree (cholangiogram) is performed via the tube.
Special procedures: Other
Fistulogram/Sinogram
Fistulogram/Sinogram are examinations used to diagnose and assess the size and shape of fistulas and sinuses and prepare a treatment plan.
- Contrast agent is injected into an opening in the body called a
- Fistulas usually involve hollow organs like the intestines, bladder, urethra and vagina. They often form as a result of infection or inflammation related to surgery, injury or radiation therapy.
- Fistulograms may also be used to assess abscess collections post-drainage and to determine whether there is a persistent communication from the collection to any surrounding structures.
- A sinogram assesses a passage called a sinus that originates or ends in one opening, often on the skin.
- Sinuses can occur throughout the body and may be related to infection or injury. Symptoms may be mild, such as a discharge of clear fluid from the skin, or more serious, such as abscess formation. A sinogram can show the extent of the problem and help develop a plan for future care.
Cystograms/urethrogram
Cystograms/urethrogram exam used to visualize the urinary bladder and/or the urethra. Contrast media is injected to fill the bladder using a urinary catheter and X-ray imaging is performed.
Video urodynamics
Video urodynamics performed by the Urologist. Video Urodynamics is the study of pressure and flows in the lower urinary tract (the bladder and tube through which you pass urine). Contrast media is injected to fill the bladder, while the pressure and flow are measured during imaging.
Video fluoroscopic Swallowing Study (VFSS)
This study is done in the X-ray department by the Speech-Language pathologist and a technologist. You will be given different foods and drinks mixed with barium. The barium makes the food and liquid show up on the x-ray.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
A procedure done by a Gastroenterologist used to find and treat problems in your pancreas, bile ducts and gallbladder. Contrast is injected and X-ray images are taken during this procedure.
Hysterosalpingogram (HSG)
This study is done in the X-ray department by a Gynecologist and technologist. It is an X-ray procedure that looks at the inside of the uterus and fallopian tubes. Contrast media is injected through a thin catheter and then X-ray images are taken.
When will I get my results?
The report of your study will be sent to your doctor as soon as it is completed.
At times, the Medical Imaging department might contact you directly, in case of concern or to have part of the study repeated or complemented.
Contact your health care provider or the Medical Imaging department if you do not receive a report of your results within 30 days to discuss the results with you.
Last updated on: October 5th, 2020


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.