Psychosis is a health condition that can be challenging to deal with alone.
Neurological symptoms like hallucinations, delusions and paranoia can make it hard to distinguish between what’s real and not — which can, in turn, make seeking treatment for yourself or a loved feel overwhelming.
To help lessen this load, The Ottawa Hospital runs a program for young adults between the ages of 16 to 35 experiencing their first episode of psychosis — the only service of its kind in the Champlain region.
Celebrating its 20th anniversary this year, the OnTrack: Champlain District Regional First Episode Psychosis Program is a voluntary rehabilitative program that reduces barriers to accessing care for psychotic disorders, ensuring individuals get the support they need as soon as possible.
One way that OnTrack does this is by using an open referral system. This means anyone can call and refer themselves, or someone they know, to the program — no family doctor or ER visit required.
“People can be afraid to seek help,” says Kaywana Malcolm, a registered nurse and a member of OnTrack’s multidisciplinary health-care team. “Because you can self-refer, we’re removing one of those major barriers.”

The importance of early intervention
Psychosis often emerges in late adolescence or early adulthood — a period when the brain is still maturing and may be more vulnerable to stress and neurobiological disruption,” explains Dr. Mary Marquardt, a neuropsychologist with the OnTrack program since 2011. “If you’re experiencing symptoms of psychosis, it’s important to get help as soon as possible to avoid any long-term cognitive, behavioural, emotional and functional impacts.”
Early intervention is also critical because successfully treating psychosis is a marathon, not a sprint. For example, it can take weeks just to find the right medication, at the right dose, with minimal to no side effects, to manage someone’s symptoms.
As a result, everyone admitted into the OnTrack program is followed for up to three years by a dedicated multidisciplinary team of health-care professionals — including dieticians, nurses, occupational therapists, psychologists, psychiatrists, recreational therapists and social workers — all working together to develop effective, long-term treatment plans for their clients.

A whole-body approach to cognitive health
Medication and symptom management are just one part of OnTrack’s approach to cognitive health. Therapeutic group interventions, art therapy and a peer support program are all offered with the goal of equipping clients — and their loved ones — with the education and support they need to feel more like themselves again and get back to their day-to-day lives.
“After three years, you really get to know your clients and their families,” says Julie Daly, a registered nurse who’s been with the program since its launch in 2005. “Sometimes they’ll call after they’ve left the program and let us know how they’re doing — that they’re heading to university or starting a new job.”
Julie notes that there is unfortunately still a lot of social stigma around psychotic disorders, which can make it hard for people to come to terms with their diagnosis.
“You just don’t hear all the stories about people with psychosis or schizophrenia going on to achieve their short-term and long-term goals, like returning to school and completing their educations, securing employment and having fulfilling relationships,” she says. “But we celebrate those successes with our clients all the time.”
Learn more about OnTrack: Champlain District Regional First Episode Psychosis Program.


Support patient care and research at
The Ottawa Hospital
You might also like…
A new guide to navigating your mental health
The Ottawa Hospital has partnered with YouTube to create an important series of videos where health-care professionals offer expert guidance to help you or a loved one navigate mental health challenges.
Ask Masi: A new support tool for front-line perinatal care providers
Parents will often describe welcoming a new child as one of the happiest times of their lives. But physicians, midwives, nurses and others on the front lines will tell you that this is not always the case for their patients. A new service for care providers called Ask Masi is here to help.
Mental health professionals and paramedics team up to help people in crisis
Seven days a week, a mental health professional from The Ottawa Hospital hits the road with a paramedic from the Ottawa Paramedic Service. Together, they respond to 911 calls for mental health emergencies across the city. Social worker Cindy Gill and paramedic Scott Farrell share how the Mental Wellbeing Response Team provides quality care for patients out in the community.
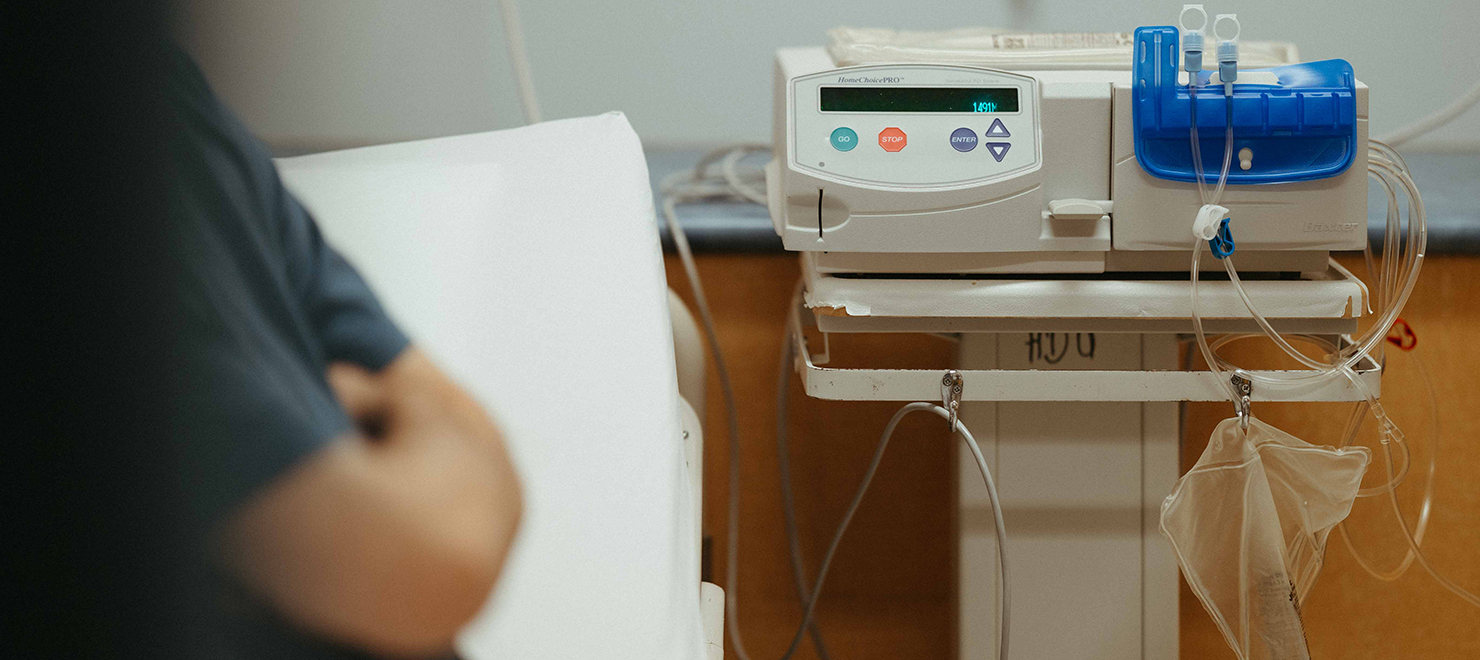
The comfort of home: Home Dialysis Program empowers patients to live more independent lives
For people living with kidney failure, the most ideal form of dialysis treatment is done in the place where they are most comfortable—their home. Five years ago, we transformed our Home Dialysis Program, enhancing quality of life for our patients, welcoming more patients, and turning it into a model for dialysis programs across the province.
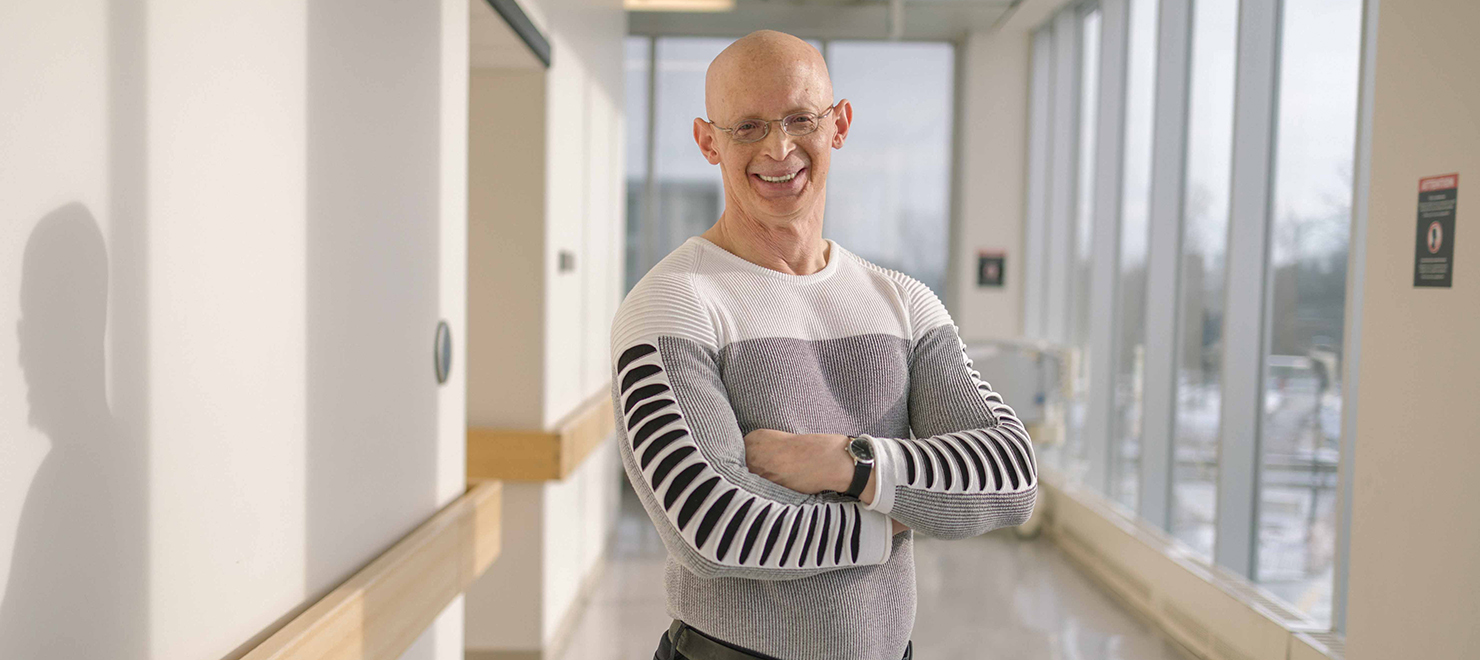
New Research Chair in Gay Men’s Health is setting out to break down barriers to care
As both a researcher and a gay man, Dr. Paul MacPherson knows all too well the stigma that gay men often face in the health-care system. Now, as the Clinical Research Chair in Gay Men’s Health at The Ottawa Hospital and the University of Ottawa, he’s on a mission to make quality health care more accessible to this often overlooked patient population.
Our mental health team is growing to meet the need for better access to care
We hear it almost every day: people in our community need better access to mental health care. The Ottawa Hospital has recruited 20 new psychiatrists since October 2020 to meet this ever-growing demand. In this article, meet four of our new team members who have come from around the world.


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.