
RN Danny Sutton-Long (left) and Respiratory Therapist Peter Eifert (right) help set up Greg Hug for one of his many daily ‘pacing’ sessions. He’s training his diaphragm to use an implanted pacemaker, which lets him breathe without using a ventilator. Eventually it will allow him to leave the Intensive Care Unit.
Greg Hug’s first breaths using his newly implanted diaphragmatic pacemaker were tough. He tired quickly, he felt breathless, and he was disappointed that he lasted only 2.5 minutes off the ventilator.
But he’s been training his diaphragm and getting stronger every day since July 25 when he underwent the ground-breaking surgery at The Ottawa Hospital.
“It’s progressing much faster than anticipated,” said Hug, a patient in the General Campus Intensive Care Unit who has been dependent on a ventilator ever since a body surfing accident in February resulted in quadriplegia. By the end of August, he was using the pacemaker for up to 570 minutes per day, in many sessions. “I’m very pleased.”
“The initial results are quite promising,” said Dr. James Villeneuve, the thoracic surgeon who performed the surgery under the direction of Dr. Raymond Onders from Case Western Reserve University in Cleveland, Ohio. Diaphragmatic pacemakers have been around in various forms for 30 years, but did not work well until Dr. Onders improved the technology. He travels the world teaching the surgery now. Although some have been implanted elsewhere in Canada, this was the first at The Ottawa Hospital.
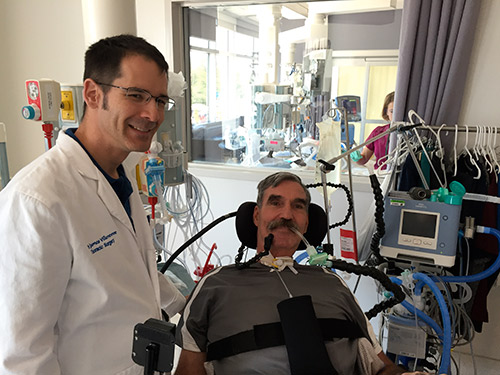
Dr. James Villeneuve, thoracic surgeon, implanted Greg Hug’s diaphragmatic pacemaker during the July 25 surgery.
Initially used with ALS patients, the pacemaker consists of a small box that the patient wears in a harness on the right side. The box is attached to pacing wires that are placed during laparoscopy through the abdominal wall and into the diaphragm. The device provides electrical stimulation that contracts the diaphragm, allowing the patient to draw breath in a way that’s similar to natural breathing.
“Technically, it is not a difficult procedure – the challenge was the order of operations, the unfamiliar equipment, where to best place the pacing leads, and how to program the pacemaker,” said Dr. Villeneuve.

Greg Hug wears the diaphragmatic pacemaker in a harness. The device is attached to pacing wires that go through the abdominal wall and into the diaphragm, delivering electrical impulses. As he trains his diaphragm, he can breathe without a ventilator for more minutes per day, and his lung capacity and oxygen saturation levels increase.
Hug can’t leave the ICU until he can get off the ventilator – the pacemaker should give him that freedom and help him avoid institutional care, said Intensivist Dr. John Kim, who has coordinated Hug’s care in the ICU.
“The surgery was a unique challenge and rewarding too, to see that you can make such a difference to his independence,” said Dr. Villeneuve. “It also opens the door for other interesting questions about weaning patients from ventilators. As we see the technology evolve to temporary wires, we may be able to use them to avoid long-term intubation or help get people out of ICU sooner. It’s an exciting avenue of research we’ll follow as the technology evolves.”

Comment on this post
Support patient care and research at
The Ottawa Hospital


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.
Is this technology available in nova scotia? My sister is a ventilator dependent quadrapelic living in ICU post injury. We are very afraid she is losing hope and her family is desperate for options.