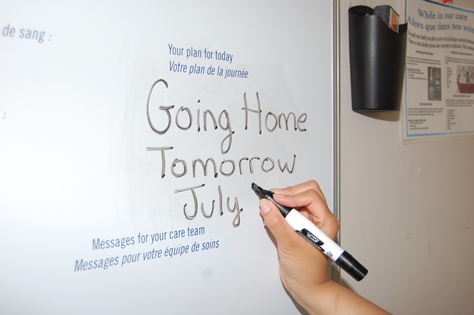
Writing the expected date of discharge on care boards in patient rooms is a key ingredient of a good discharge process.
Patient Advocacy heard from a patient’s family that, after receiving great care, their loved one was discharged without enough notice and without enough home support in place. The patient was worried she might have to be admitted again.
“This underlines why The Ottawa Hospital’s discharge process needs a makeover,” said Karen Nelson, Chief of Social Work. She and Cheryl Geymonat, Corporate Emergency Department Project Manager, are guiding the changes being planned to improve the process on every inpatient unit.
“In this case, the patient’s and family’s perception of their care is altered by the unpleasant way they left the hospital,” said Nelson. “It’s like if you go to a restaurant and really enjoyed the meal, but then you got your bill late, there were mistakes on it, and then you got a parking ticket. When you look back on the fine meal, it’s not a fine meal any more.”
The discharge process is among the top five complaints received by Patient Advocacy and most of them boil down to a lack of communications – with the family, with the doctors, with long-term-care homes and more.
The goal is to standardize the discharge process to make the transition as safe as possible, with clearly identified roles and accountabilities that will be sustainable. The key is communications – so everyone not only knows what their responsibilities are, but also when to take action.
“If the plans for post-discharge care are poorly communicated, the likelihood patients will come back is higher,” said Geymonat.
Indeed, research in 2004 by Dr. Alan Forster showed that 25 percent of all patients have an adverse event after discharge (often related to medication), and 50 percent of those adverse events could have been improved or prevented.
Geymonat and Nelson are guiding the changes using the LEAN framework – made famous by Toyota but used in health care for more than 20 years – to streamline and simplify the discharge process, looking for many small changes that will add up to a big solution, such as simplifying forms, consistently posting discharge dates on care boards, planning for discharge upon admission, and reducing bottlenecks in patient flow.
“Our occupancy is very high between 11 a.m. and 3 p.m.,” said Nelson. “New patients have come in but few patients have left. For those who are going to be discharged, we need to have them prepared and able to leave early in the day.”
The first stage of fixing the process – diagnosing the problem – is complete and they’re now assembling frontline staff to help design the solution. Watch for updates.
“It’s so exciting because there are many possible solutions that should improve patient satisfaction as well as staff satisfaction,” said Geymonat.
7 benefits to a good discharge process
Research shows that a good discharge process will:
- Reduce distress and improve satisfaction for patients and families
- Ensure clear follow-up care and medication orders
- Reduce rehospitalisation rates
- Reduce length-of-stay rates
- Reduce wait times for acute-care beds
- Improve patient flow through the hospital
- Help manage hospital resources efficiently and effectively
Inpatients discharged by 11 a.m.:
Goal: 30%
TOH now: average of 22% but some units as low as 11%
Complaints:
139 complaints – 8% of total complaints – received by the Department of Patient Advocacy in 2013-14 were related to the discharge process.

Support patient care and research at
The Ottawa Hospital


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.