toh
Special Conditions
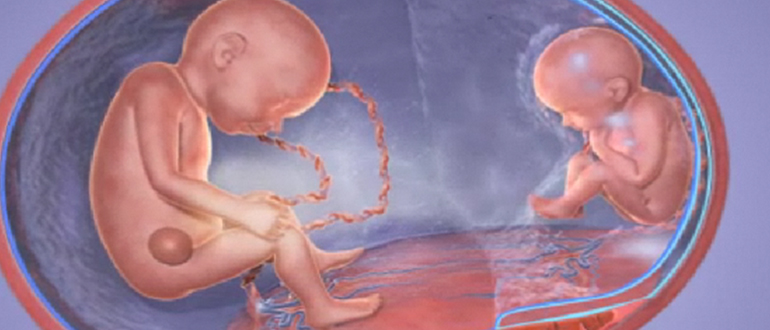 MC twins will develop twin-twin transfusion syndrome (TTTS). In this condition, blood vessels from each baby travel through the umbilical cord into the placenta, where they connect with each other. These special blood vessels (called anastomoses) carry blood in only one direction. This leads to one fetus becoming a blood donor for the other fetus (the blood recipient). When this situation develops, it can lead to an imbalance in the amount of amniotic fluid seen on ultrasound in each babies’ sac. This is called poly/oli, where the recipient fetus has too much amniotic fluid, called polyhydramnios or poly for short, whereas the donor fetus, donating its blood to its co-twin, stops producing much amniotic fluid and develops oligohydramnios (oli for short) or lack of amniotic fluid. This syndrome most often will develop in the second trimester but can be detected even in the early third trimester. There are several stages to this disease. If your doctor detects this condition on your regular bi-weekly ultrasound, they may recommend fetal treatment to stop the net flow of blood from one fetus to the other. This is accomplished by laser therapy to block the vessels causing the problem. This procedure is offered at the provincial referral center at Mt. Sinai Hospital in Toronto. Following the laser therapy, you will return to TOH for frequent monitoring until you have your babies.
MC twins will develop twin-twin transfusion syndrome (TTTS). In this condition, blood vessels from each baby travel through the umbilical cord into the placenta, where they connect with each other. These special blood vessels (called anastomoses) carry blood in only one direction. This leads to one fetus becoming a blood donor for the other fetus (the blood recipient). When this situation develops, it can lead to an imbalance in the amount of amniotic fluid seen on ultrasound in each babies’ sac. This is called poly/oli, where the recipient fetus has too much amniotic fluid, called polyhydramnios or poly for short, whereas the donor fetus, donating its blood to its co-twin, stops producing much amniotic fluid and develops oligohydramnios (oli for short) or lack of amniotic fluid. This syndrome most often will develop in the second trimester but can be detected even in the early third trimester. There are several stages to this disease. If your doctor detects this condition on your regular bi-weekly ultrasound, they may recommend fetal treatment to stop the net flow of blood from one fetus to the other. This is accomplished by laser therapy to block the vessels causing the problem. This procedure is offered at the provincial referral center at Mt. Sinai Hospital in Toronto. Following the laser therapy, you will return to TOH for frequent monitoring until you have your babies.
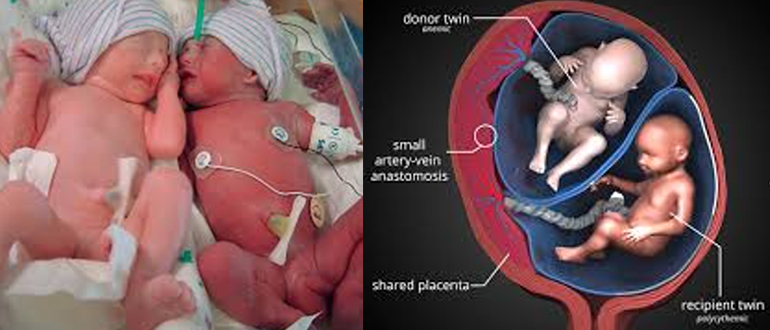 Twin Anemia-Polycythemia Sequence or TAPS is also a special condition in MC twins, whereby there is a slow transfusion of blood from one fetus to the other. Like TTTS, it is due to the presence of communicating blood vessels in the placenta, but these vessels are usually smaller in size and fewer in number than in TTTS. The result is that one baby can become very anemic while the other develops very thick blood with a high hemoglobin. Neither of these situations is good in the long term. Fortunately, this condition develops spontaneously in only about 5 percent of MC twins. It is more frequently encountered after laser therapy for TTTS (about 11 percent) when very tiny connecting blood vessels, about a 1 mm in caliber, are not blocked during laser treatment. Treatment of this condition may include blood transfusion before birth (intrauterine transfusion) to one baby, to correct the anemia and improve the oxygen supply. The other twin may need to have some of the very thick blood removed before birth and replaced with a saltwater solution (saline) to thin the baby’s blood.
Twin Anemia-Polycythemia Sequence or TAPS is also a special condition in MC twins, whereby there is a slow transfusion of blood from one fetus to the other. Like TTTS, it is due to the presence of communicating blood vessels in the placenta, but these vessels are usually smaller in size and fewer in number than in TTTS. The result is that one baby can become very anemic while the other develops very thick blood with a high hemoglobin. Neither of these situations is good in the long term. Fortunately, this condition develops spontaneously in only about 5 percent of MC twins. It is more frequently encountered after laser therapy for TTTS (about 11 percent) when very tiny connecting blood vessels, about a 1 mm in caliber, are not blocked during laser treatment. Treatment of this condition may include blood transfusion before birth (intrauterine transfusion) to one baby, to correct the anemia and improve the oxygen supply. The other twin may need to have some of the very thick blood removed before birth and replaced with a saltwater solution (saline) to thin the baby’s blood.
 Selective intrauterine growth restriction (sIUGR) in twins also affects approximately 15 % of MC twins. Usually there is a significant difference (discordance) in the estimated fetal weights of twins on ultrasound assessment. In addition, one fetus will have an estimated weight that is below the 10th centile. That means that over 90 percent of all babies assessed on ultrasound will have an estimated weight that exceeds that of the smaller baby. Unlike TTTS, there is usually no big discrepancy in the volume of amniotic fluid around each baby. Once this condition is suspected, the doctors will look carefully at the pattern of blood flow going through the artery in the umbilical cord. Different patterns of blood flow have been associated with differences in outcome, in terms of survival and gestational age at which the twins are born.
Selective intrauterine growth restriction (sIUGR) in twins also affects approximately 15 % of MC twins. Usually there is a significant difference (discordance) in the estimated fetal weights of twins on ultrasound assessment. In addition, one fetus will have an estimated weight that is below the 10th centile. That means that over 90 percent of all babies assessed on ultrasound will have an estimated weight that exceeds that of the smaller baby. Unlike TTTS, there is usually no big discrepancy in the volume of amniotic fluid around each baby. Once this condition is suspected, the doctors will look carefully at the pattern of blood flow going through the artery in the umbilical cord. Different patterns of blood flow have been associated with differences in outcome, in terms of survival and gestational age at which the twins are born.
Fetal loss in MC twins occurs more often than in DC twins. At times, it is clearly linked to one of the special MC twin conditions discussed above. Many times, it is unanticipated and not predictable, even with intensive ultrasound monitoring and clinic visits every two weeks throughout the pregnancy. It is estimated that the fetal loss rate of one or more MC twins after 34weeks, can be as high as four percent, despite intensive monitoring. The only strategy for prevention of this adverse event is to electively deliver all MC twins prematurely around 34 weeks. If this policy were to be adopted universally, it would lead to a higher incidence of prematurity-associated problems and our intensive care nurseries would be overfull. To reduce the incidence of late fetal death we currently electively deliver MC twins at or around 36 weeks with intense fetal monitoring before this time.
The consequence of MC fetal death in utero from any cause is that it places the co-twin at 12 percent risk of subsequent fetal death as well. Even if the co-twin survives, the death may lead to significant problems with neurodevelopment in the survivor. This is caused by loss of blood from the surviving twin towards the dying fetus, leading to decreased blood flow to the brain and potential brain damage in about 30 percent of cases. The severity of this effect depends on what time in pregnancy the fetal death occurs and is more likely to be a problem if the fetal loss occurs in the later second or third trimester. Should one fetus be lost early in the pregnancy, your doctor may not recommend early delivery of the other fetus as the potential damage to the survivor happens at the time of the fetal loss.
Twin Reversed Arterial Perfusion Sequence or TRAP is a very rare MC twin condition, occurring in only about 1/35,000 pregnancies. In this condition one fetus develops normally while the other has severe structural differences. The baby with normal structure (often referred to as the “Pump” twin) pumps blood to the other fetus (the “Perfused” twin). As a result, its heart works overtime to support its co-twin.
Blood with low oxygen is pumped as it leaves one baby, with all the waste products to the other through a single artery connecting the babies. The baby receiving the blood with low oxygen will not develop normally and has no developed heart structures, relying entirely on its co-twin for survival. Heart failure can develop in the structurally normal twin. If this condition is diagnosed, your doctor will present several options for management to improve the chance of survival of the Pump twin. The structural differences in the co-twin are severe and incompatible with life.
Conjoined twins, or Siamese twins as they may be known, are also very rare findings in twins. With the uptake of first-trimester ultrasound screening, they are often detected early in the pregnancy. In the most severe cases, these fetuses share structures such are hearts or livers, making separation of the twins after birth very difficult or impossible. Pregnancy-related complications, including fetal loss or preterm birth, are also frequent in these cases. The success of attempted separation, if potentially possible, depends on many factors and involves detailed assessment by many different specialties and these pregnancies are evaluated in Toronto.
Last updated on: April 29th, 2021


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.