
Patient Johann Moennich (centre) and his partner, Ursula Robitschek (right), have recommended the Champlain – Falls Assessment and Streamlined Treatment Clinic to their friends. Physiotherapist Mary Haller (left) assesses patients in the clinic, along with a nurse, geriatrician and pharmacist.
Johann Moennich crossed his arms and slowly stood up from the chair, to demonstrate his balance and strength to Physiotherapist Mary Haller.
Ursula Robitschek, Mr. Moennich’s partner, later reported that he’d been doing his falls-prevention exercises daily and following other recommendations he’d received in the Champlain – Falls Assessment and Streamlined Treatment (C-FAST) Clinic.
Haller assesses patients in the clinic on Monday and Thursday afternoons, along with an advanced practice nurse, geriatrician and pharmacist.
The team assesses patients for fall risk factors, including multiple medications; dropping blood pressure upon standing; muscle weakness; balance issues; pain; improper footwear; reduced vision; and unsafe home environments. Then, the team initiates treatment and makes recommendations.

Physiotherapist Mary Haller (right) tested patient Johann Moennich’s balance and strength, while his partner, Ursula Robitschek, watched carefully.
“If we can see patients early in their ‘falls history,’ we can help them modify their risk factors, which can help reduce the number of falls and injuries they might otherwise have,” said Geriatrician Dr. Shirley Huang. “We want to help them stay independent longer and hopefully avoid hospital admissions due to injuries from falls.”
Some sobering numbers triggered the creation of the falls clinic, which began as a pilot in October 2015 and became permanent in spring 2016:
- In 2013, the Champlain region had 2,764 falls-related hospitalizations, which cost an estimated $17.2 million to treat.
- In 2014-2015, TOH’s two Emergency Departments saw 4,665 seniors who had fallen.
- In 2015, the Champlain region ranked second highest in Ontario for falls resulting in ED visits and the highest for falls-related hospitalizations.
“We’re being proactive in targeting this high-risk population,” said Advanced Practice Nurse Taryn Mackenzie.
Referrals are currently accepted from specialized geriatric services. A mobile falls clinic will soon be trialled at a family health team clinic and retirement home. The goal is to create a model that can be adopted by other health-care teams in the region.
After Mr. Moennich was assessed, he was advised to use a straight cane and wear proper shoes, had his medications changed to reduce his back pain, was given information on keeping hydrated to avoid dizziness when he stands, and received a specialized home exercise program and home safety information.
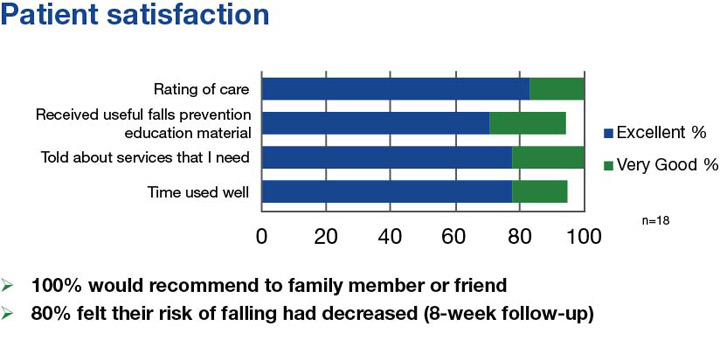
An evaluation survey found that 100 percent of those who referred patients to the clinic would do so again. Feedback from patients has also been excellent.
“The whole setup of this clinic was such a positive experience,” said Mrs. Robitschek. “It’s a highly recommended program and it’s really quite exciting to know it’s available for seniors who need this kind of support.”
“The staff treated me well,” added Mr. Moennich.
Currently, about 30 percent of seniors fall each year. Falls are both predictable and preventable. Paying attention to the numerous factors that contribute to seniors’ falls can help reduce their risk of future falls.
Seniors can use the Staying Independent Checklist to assess their own risk factors for falls and then discuss them with their doctor.
For more information and falls-related resources, see the Champlain Falls Prevention Strategy, and the Regional Geriatric Program of Eastern Ontario.

Support patient care and research at
The Ottawa Hospital


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.