
CANVent Respiratory Therapist Kathy Walker helped Marty Meech learn how to use his noninvasive ventilator at home.
Marty Meech eyes the small square machine on his living room coffee table. It is key to his independence because it will help him breathe.
Meech was diagnosed with Amyotrophic Lateral Sclerosis (ALS) 5.5 years ago. This wasting disease, caused by the gradual death of the nerves that control the muscles, slowly paralyzes such patients so they cannot walk, swallow or breathe.
Meech initially carried on with his life after diagnosis, working at Pepsi. However, after suffering a blood clot in his lungs in November 2016, followed by inflammation around his heart, Meech’s breathing became seriously impaired. He needed a ventilator upstairs in his bedroom at night to help him breathe. He could no longer work and had to retire, spending his days in his Barrhaven home.
Recently, Meech’s breathing became more difficult during the day, which is why he has a ventilator sitting on his coffee table. He puts the ventilator tube’s mouthpiece in his mouth and takes a deep breath.
“I’ve been going upstairs at nine o’clock and going to sleep early because I need the breathing machine,” said Meech. “Whereas now, with this new ventilator I can stay down here and watch TV, talk to my family, or go outside. I should gain so much more independence – freedom to do other things.”

Having a ventilator available 24 hours a day helps Marty Meech, who has ALS, live comfortably at home.
When Meech had his last assessment at the CANVent Clinic, Dr. Douglas McKim, Medical Director of the CANVent Program, recommended that Meech use a second ventilator during the day.
Equipment was ordered from the Ontario Ministry of Health Ventilator Equipment Pool and delivered to his house. Then Respiratory Therapist Kathy Walker visited Meech at home to set it up and teach him how to use it. This makes it easier for patients like Meech, who no longer need to go to the clinic in The Ottawa Hospital Rehabilitation Centre, to learn about the equipment and set it up correctly themselves at home.
Usually, when neuromuscular patients have 24-hour breathing issues, they receive what’s called a tracheostomy – a tube called a ‘surgical airway’ is inserted in their windpipe and hooked up to a ventilator, to help them breathe. However, once patients have a tracheostomy, they often remain in hospital because of the complex care required.
Tracheostomies are still widely performed at health centres across Canada for long-term ventilation.
In 2008, the Ontario Ministry of Health found that about 25 percent of long-term ventilated patients in Toronto had tracheostomies. In London it was 35 percent. In Ottawa it was only 4 percent. The noninvasive approaches in the CANVent program, including mouthpiece ventilation, likely contribute to these differences.
“It was developed here at The Ottawa Hospital really out of a need,” said Dr. McKim, “At the Rehabilitation Centre, we would see all patients in the region with challenging neuromuscular disorders. And nobody was really looking after their respiratory issues, which can be the major cause of mortality. For example, with ALS, 85 to 90 percent of patients die of respiratory failure, so respiratory care is critical.”
“We can provide 24-hour ventilation noninvasively to large numbers of patients, so they don’t need a tracheostomy. They don’t need surgery. Plus, they do not get all the complications that go along with tracheostomy care. And patients can stay at home.”
In 1993, Dr. McKim set up a program that offered patients with serious respiratory complications, noninvasive (nonsurgical), supports to help them breathe. Since then, for example, no patients at The Ottawa Hospital with Duchenne Muscular Dystrophy have had permanent tracheostomies.
In 2012, the program became CANVent, an acronym for Canadian Alternatives in Noninvasive Ventilation. Doctors refer patients who may be at risk for respiratory complications to the program. This includes patients with ALS, muscular dystrophy, spinal cord injury, multiple sclerosis, post-polio syndrome and many others.
“We can identify patients at risk and reduce the likelihood of them having to come to the Emergency Department, or worse the ICU [intensive care unit], and having tracheostomy invasive ventilation. That is our raison d’être,” said Dr. McKim, who has delivered more than 30 international presentations about noninvasive airway management.
The CANVent Program has between 600 and 700 patient visits each year, including about 150 new consultations.
“It’s an opportunity for patients to gain more autonomy and an opportunity to become more independent,” said Walker. “We can provide 24-hour ventilation noninvasively to large numbers of patients, so they don’t need a tracheostomy. They don’t need surgery. Plus, they do not get all the complications that go along with tracheostomy care. And patients can stay at home.”
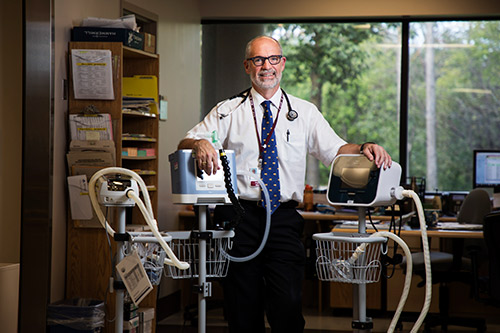
“Critical Care Services Ontario visited us in February 2016, because Ottawa had a lower rate of long-term invasive ventilation in the ICU and in the community, to see what we were doing that was unique,” said Dr. Douglas McKim, Medical Director of the CANVent program, the sleep program at The Ottawa Hospital, and Professor of Medicine at the University of Ottawa. “We’re saving costs while also improving the life quality and survival of individuals with neuromuscular disorders.”
Dr. McKim pointed out that The Ottawa Hospital is one of the few centres in the country that has expertise in mouthpiece ventilation and has published the experience. “Every patient who is on a mouthpiece, versus the tracheostomy, is probably saving the health-care system $200,000 a year.”
Often, patients who have a tracheostomy remain in hospital or long-term care for the rest of their lives, some entirely in ICU. Dr. McKim said one patient was referred from Toronto who was told he needed a tracheostomy. He was given a noninvasive ventilator and mouthpiece at the CANVent clinic and didn’t need a tracheostomy for 11 years. Dr. McKim calculated that this case alone likely saved the health-care system $2.2 million.
“Not only is this remarkably cost-effective and improves patients’ quality-of-life,” said Dr. McKim, “but patients feel better because they are not attached to a tracheostomy. Their lives are less complicated. They have fewer hospitalizations as a result.”
The CANVent program is sharing this knowledge with practitioners around the country, and the world, so that neuromuscular patients like Marty Meech do not have to suffer the fate of preventable respiratory failure and ICU admission.

Support patient care and research at
The Ottawa Hospital
You might also like…
A volunteer program that taps into the power of music
Studies have shown that music can benefit the body, mind, relationships and community. Musical Moments is a program where volunteers play live music to support positive outcomes for patients, visitors and staff.
We’ve got you covered: The Ottawa Hospital now offers bandages for a variety of skin tones
Whenever you’ve scraped your knee or had your blood drawn, odds are your bandage was the same colour every time. Peach has been the default hue for over a century — but no longer at The Ottawa Hospital.
New gender-affirming surgery clinic now accepting patients
The Ottawa Hospital’s new gender-affirming surgery clinic is truly one of a kind. Launched in September 2023, it’s the only clinic in Ontario to offer trans and non-binary patients facial, top and bottom procedures. Plastic Surgeon Dr. Nicholas Cormier and his team are happy to announce that they are now accepting patient referrals from physicians.
Patient gifts a piece of home to Indigenous Cancer Program
Inuit patients can now see and hold a piece of their traditional territory in the Windòcàge Room at the General Campus, thanks to an interactive gift donated to The Ottawa Hospital by a cancer patient.
Mental health professionals and paramedics team up to help people in crisis
Seven days a week, a mental health professional from The Ottawa Hospital hits the road with a paramedic from the Ottawa Paramedic Service. Together, they respond to 911 calls for mental health emergencies across the city. Social worker Cindy Gill and paramedic Scott Farrell share how the Mental Wellbeing Response Team provides quality care for patients out in the community.
Second Chance: Don’s song for the people who saved his life
Making music has always been a big part of Don’s life, so when the staff and doctors at The Ottawa Hospital saved him from the brink of death, he could think of no better way to thank them.


 To reset, hold the Ctrl key, then press 0.
To reset, hold the Ctrl key, then press 0.






Comment on this post